Living with gastroparesis can feel overwhelming, especially when eating — something that should nourish and energize you — becomes a source of discomfort. Nausea, bloating, early fullness, reflux, and abdominal pain can make even small meals difficult. Fortunately, a well-structured Gastroparesis Diet Plan can significantly reduce symptoms and improve quality of life.
This comprehensive guide explains what gastroparesis is, how diet impacts symptoms, and most importantly, what to eat and avoid when following a Gastroparesis Diet Plan.
What Is Gastroparesis?
Gastroparesis, also called delayed gastric emptying, is a condition in which the stomach empties food into the small intestine more slowly than normal. Unlike other digestive disorders, there is no physical blockage — instead, the stomach muscles or nerves do not function properly.
One of the most common causes is long-term diabetes, which can damage the vagus nerve. Other causes include viral infections, certain medications, abdominal surgery, and neurological conditions. In some cases, the cause is unknown (idiopathic gastroparesis).
Common symptoms include:
- Nausea
- Vomiting undigested food
- Bloating
- Early satiety (feeling full quickly)
- Acid reflux
- Abdominal pain
- Weight loss or malnutrition
Because the stomach empties slowly, the type and texture of food you eat directly impact how severe your symptoms become. That’s why a structured Gastroparesis Diet Plan is one of the most important parts of treatment.
Why a Gastroparesis Diet Plan Is Essential
The main goal of a Gastroparesis Diet Plan is to:
- Improve stomach emptying
- Reduce nausea and vomiting
- Prevent dehydration
- Maintain adequate nutrition
- Stabilize blood sugar levels (especially for diabetics)
Certain foods — particularly those high in fat and fiber — slow stomach emptying even further. Others are harder to digest and may form bezoars (hardened masses of undigested food).
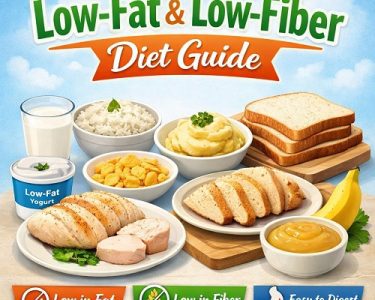
A proper Gastroparesis Diet Plan focuses on:
- Low-fat foods
- Low-fiber options
- Soft or liquid textures
- Smaller, more frequent meals
General Guidelines for a Gastroparesis Diet Plan
Before diving into specific foods, here are foundational rules that most doctors and dietitians recommend:
1. Eat Small, Frequent Meals
Instead of three large meals, aim for 5–6 small meals per day. Smaller portions empty from the stomach more easily.
2. Choose Soft or Liquid Foods
Liquids leave the stomach faster than solid foods. Soups, smoothies, purees, and blended meals are often better tolerated.
3. Reduce Fat Intake
Fat slows gastric emptying. However, small amounts of liquid fats (like oils in soups) may be tolerated better than solid fats.
4. Limit Fiber
Fiber slows digestion and can form bezoars. Avoid raw vegetables, skins, seeds, and tough plant fibers.
5. Chew Thoroughly
Chewing food well reduces the workload on your stomach.
6. Sit Upright After Eating
Remain upright for at least 1–2 hours after meals to promote digestion and reduce reflux.
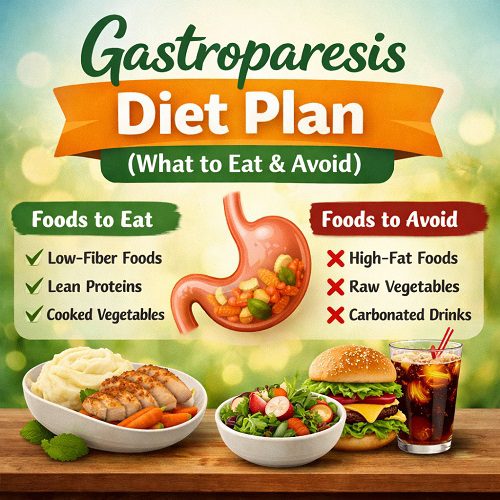
What to Eat on a Gastroparesis Diet Plan
The best foods for a Gastroparesis Diet Plan are easy to digest, low in fat, and low in fiber.
1. Refined Grains
These are easier to digest than whole grains.
Good options include:
- White bread
- Plain bagels
- White rice
- Pasta
- Low-fiber cereals
- Crackers
Avoid whole-grain and high-fiber versions.
2. Lean Protein Sources
Protein is essential to prevent muscle loss and malnutrition.
Better choices:
- Skinless chicken
- Turkey
- Lean ground beef
- Fish
- Eggs
- Egg whites
- Tofu
- Smooth nut butters (in small amounts)
If solid meats are difficult to tolerate, try:
- Ground meats
- Shredded meats
- Blended soups with protein
- Protein shakes
3. Low-Fiber Fruits
Fruits should be peeled, cooked, or canned.
Best options:
- Applesauce
- Canned peaches or pears (without skin)
- Ripe bananas
- Melons
- Fruit smoothies (without seeds or skins)
Avoid raw apples, berries, oranges, and fruits with seeds or tough skins.
4. Well-Cooked Vegetables
Raw vegetables are usually difficult to digest.
Better choices include:
- Cooked carrots
- Zucchini (peeled)
- Green beans (well-cooked)
- Pumpkin
- Mashed potatoes (without skin)
Vegetables should be soft enough to mash with a fork.
5. Dairy (If Tolerated)
Some people tolerate low-fat dairy well.
- Skim milk
- Low-fat yogurt
- Cottage cheese
- Pudding
If lactose intolerance is present, choose lactose-free options.
6. Soups and Broths
Soups are often ideal in a Gastroparesis Diet Plan because they combine hydration and nutrition in an easily digestible form.
- Chicken noodle soup
- Cream-based soups (low-fat)
- Pureed vegetable soups
- Bone broth
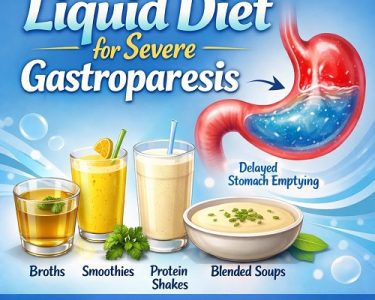
7. Liquid Nutrition
When symptoms are severe, liquids are often best tolerated.
Options include:
- Meal replacement shakes
- Protein smoothies
- Nutritional supplements (as recommended by a healthcare provider)
Liquids empty from the stomach more efficiently than solids, making them crucial during flare-ups.
What to Avoid on a Gastroparesis Diet Plan
Certain foods worsen symptoms by slowing digestion or increasing stomach workload.
1. High-Fiber Foods
Fiber delays gastric emptying and can form bezoars.
Avoid:
- Raw vegetables
- Corn
- Broccoli
- Cabbage
- Beans and lentils
- Whole grains
- Nuts and seeds
- Popcorn
2. High-Fat Foods
Fat slows stomach emptying significantly.
Avoid:
- Fried foods
- Fast food
- Fatty cuts of meat
- Sausage
- Bacon
- Cream-heavy dishes
- Butter in large amounts
- Full-fat dairy
Small amounts of liquid fats may be tolerated better than solid fats.
3. Tough or Fibrous Meats
Avoid:
- Steak
- Pork chops
- Processed meats
- Large chunks of meat
These are harder to digest and may sit in the stomach longer.
4. Carbonated Beverages
Soda and sparkling water can worsen bloating and pressure.
5. Alcohol
Alcohol can irritate the stomach lining and delay gastric emptying.
6. Foods That Form Bezoars
Certain foods are particularly risky:
- Persimmons
- Coconut
- Orange membranes
- Apple peels
These foods are fibrous and difficult to digest.
Sample One-Day Gastroparesis Diet Plan
Here’s an example of how a simple Gastroparesis Diet Plan might look:
Breakfast:
Scrambled eggs + white toast + applesauce
Mid-Morning Snack:
Low-fat yogurt or protein shake
Lunch:
Chicken noodle soup + saltine crackers
Afternoon Snack:
Banana or pudding
Dinner:
Baked fish + mashed potatoes (no skin) + cooked carrots
Evening Snack:
Smoothie made with skim milk and canned peaches
Meals should be small — roughly 1 to 1½ cups per serving.
Special Considerations for Diabetics
Gastroparesis is common in people with diabetes. Delayed stomach emptying makes blood sugar management more challenging because food absorption becomes unpredictable.
If you have diabetes:
- Monitor blood sugar frequently
- Work closely with your doctor to adjust insulin timing
- Avoid large carbohydrate-heavy meals
- Consider liquid meals for better glucose control
A personalized Gastroparesis Diet Plan is especially important in this case.
Tips for Managing Flare-Ups
During severe symptom periods:
- Switch to liquids temporarily
- Sip fluids slowly throughout the day
- Avoid solid foods for 24–48 hours if vomiting is present
- Stay hydrated with electrolyte solutions
- Resume soft foods gradually
If vomiting is persistent or severe, seek medical attention.
Nutritional Risks to Watch
Because food intake is often limited, people with gastroparesis are at risk for:
- Weight loss
- Dehydration
- Vitamin deficiencies (B12, iron, vitamin D)
- Protein malnutrition
Your doctor may recommend supplements or, in severe cases, feeding support.
Working with a Dietitian
Every person tolerates foods differently. A registered dietitian can customize a Gastroparesis Diet Plan based on:
- Symptom severity
- Weight goals
- Nutritional deficiencies
- Diabetes status
- Food preferences
Keeping a food journal can help identify trigger foods.
Final Thoughts
Managing gastroparesis requires patience and consistency, but the right Gastroparesis Diet Plan can dramatically reduce symptoms and improve daily life. The key principles are simple:
- Eat small, frequent meals
- Choose low-fat, low-fiber foods
- Focus on soft or liquid textures
- Avoid tough, fibrous, and fried foods
- Stay upright after eating
While diet cannot cure gastroparesis, it is one of the most powerful tools for symptom control. With careful planning and support from healthcare professionals, you can nourish your body while minimizing discomfort.
If you suspect gastroparesis or struggle with persistent digestive symptoms, consult your healthcare provider for proper diagnosis and a tailored treatment plan.
Your digestive health matters — and the right Gastroparesis Diet Plan can make all the difference.