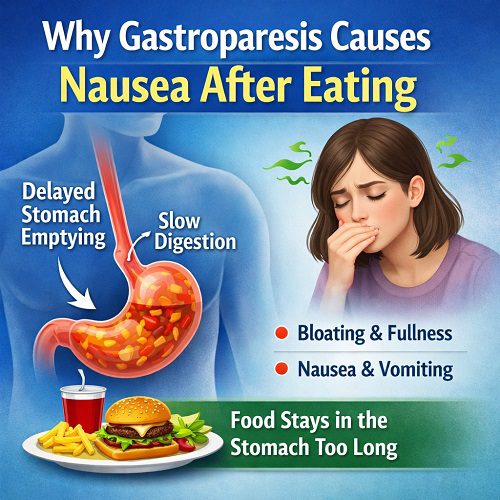
For many people, eating is a pleasurable and nourishing experience. But for individuals living with gastroparesis, meals can trigger discomfort, bloating, and persistent nausea. If you have ever wondered why Gastroparesis Causes Nausea, especially Nausea After Eating, the answer lies in how this digestive disorder interferes with the stomach’s normal function.
Gastroparesis, sometimes called delayed gastric emptying, disrupts the natural movement of food from the stomach to the small intestine. When this process slows down or stops altogether, food lingers in the stomach far longer than it should. This delayed emptying sets off a cascade of symptoms—most notably nausea.
In this comprehensive article, we will explore:
- What gastroparesis is and how it develops
- The digestive process under normal conditions
- Why Gastroparesis Causes Nausea
- Why Nausea After Eating is one of the hallmark symptoms
- Contributing factors and complications
- Treatment strategies and symptom management
- Practical dietary and lifestyle guidance
By understanding the science behind the condition, you can better manage symptoms and improve quality of life.
What Is Gastroparesis?
Gastroparesis is a chronic digestive disorder characterized by delayed gastric emptying without any physical blockage. The stomach muscles and nerves that normally contract to push food into the small intestine fail to work properly.
The stomach relies heavily on the vagus nerve to regulate muscle contractions. When this nerve is damaged or impaired, the stomach’s coordinated muscular activity weakens. As a result, food remains in the stomach longer than normal.
Common causes include:
- Diabetes (especially long-standing or poorly controlled cases)
- Post-surgical complications
- Neurological disorders
- Autoimmune conditions
- Certain medications
- Idiopathic causes (unknown origin)
Regardless of the cause, the outcome is similar: impaired stomach motility. And this is precisely why Gastroparesis Causes Nausea.
How Normal Digestion Works
To understand why Gastroparesis Causes Nausea, it helps to first understand how digestion normally functions.
Step 1: Food Enters the Stomach
After swallowing, food travels down the esophagus and enters the stomach. The stomach begins mechanical digestion by churning food and mixing it with gastric juices.
Step 2: Controlled Emptying
The stomach doesn’t empty all at once. Instead, it releases small amounts of partially digested food into the small intestine in a carefully regulated manner.
Step 3: Coordinated Muscle Contractions
Strong, rhythmic muscle contractions (peristalsis) move food toward the pylorus, the opening that connects the stomach to the small intestine.
When this system works properly, food empties in approximately 2–4 hours, depending on the meal.
But in gastroparesis, this process slows dramatically. And that delay is the key reason why Nausea After Eating becomes such a persistent symptom.
Why Gastroparesis Causes Nausea
Now let’s address the core question: why does gastroparesis cause nausea?
There are several physiological mechanisms involved.
1. Stomach Overdistension
When food lingers in the stomach, it accumulates. The stomach stretches beyond its normal capacity. This overstretching activates stretch receptors in the stomach lining, which send signals to the brain.
The brain interprets these signals as discomfort or nausea.
This is one of the primary reasons Gastroparesis Causes Nausea.
2. Abnormal Gastric Rhythms
The stomach has its own electrical rhythm, often called gastric slow waves. These waves coordinate muscular contractions.
In gastroparesis, this rhythm becomes disorganized. The result is ineffective or chaotic contractions. Instead of moving food forward, the stomach may contract in an unproductive manner.
These abnormal contractions contribute to sensations of queasiness and Nausea After Eating.
3. Food Fermentation and Gas Production
When food sits in the stomach too long, it may begin to ferment. This fermentation process produces gas and increases pressure within the stomach.
Gas buildup leads to bloating and discomfort. Increased pressure further stimulates nausea pathways in the brain.
4. Increased Sensitivity of the Gut-Brain Axis
People with gastroparesis often have heightened visceral sensitivity. This means the nerves connecting the digestive system and the brain overreact to normal stimuli.
Even small amounts of retained food can trigger disproportionate nausea signals.
Thus, Gastroparesis Causes Nausea not only because of mechanical delay but also because of increased nerve sensitivity.
5. Hormonal Imbalance
The stomach releases hormones that regulate digestion and appetite. Delayed emptying disrupts the release of these hormones.
For example:
- Gastrin
- Motilin
- Ghrelin
When these hormones are dysregulated, the digestive system loses its rhythm, contributing to persistent Nausea After Eating.
Why Nausea After Eating Is So Common
One of the most frustrating symptoms patients report is Nausea After Eating. Why does nausea worsen immediately following meals?
1. Immediate Increase in Gastric Volume
When food enters an already slow-moving stomach, volume increases quickly. If previous food hasn’t emptied, the new meal adds to the backlog.
This rapid distension intensifies nausea signals.
2. Fat and Fiber Slow Emptying Further
High-fat and high-fiber foods slow gastric emptying even in healthy individuals. In gastroparesis, these foods can dramatically worsen symptoms.
After consuming such meals, patients often experience severe Nausea After Eating.
3. Blood Sugar Fluctuations (Especially in Diabetes)
In diabetic gastroparesis, delayed stomach emptying causes unpredictable blood glucose levels. Blood sugar spikes and drops can independently trigger nausea.
Thus, in diabetic patients, Gastroparesis Causes Nausea through both mechanical and metabolic pathways.
The Role of the Vagus Nerve
The vagus nerve is central to understanding why Gastroparesis Causes Nausea.
This nerve controls:
- Stomach muscle contractions
- Secretion of digestive enzymes
- Communication between gut and brain
Damage to the vagus nerve disrupts coordinated digestion. Without proper signaling, food stagnates.
Additionally, because the vagus nerve also carries sensory information to the brain, its dysfunction can amplify nausea sensations.
Additional Symptoms That Accompany Nausea
While nausea is common, it rarely occurs alone. Other symptoms often include:
- Vomiting undigested food
- Early satiety (feeling full quickly)
- Bloating
- Abdominal pain
- Loss of appetite
- Weight loss
Vomiting often provides temporary relief because it reduces stomach pressure. This again demonstrates how Gastroparesis Causes Nausea primarily through retention and distension.
Complications of Persistent Nausea
Chronic Nausea After Eating can lead to serious complications:
1. Malnutrition
When eating triggers nausea, patients may avoid food. Reduced intake leads to vitamin deficiencies and weight loss.
2. Dehydration
Frequent vomiting causes fluid imbalance.
3. Bezoars
Undigested food can harden into masses called bezoars. These can block the stomach outlet and worsen symptoms.
4. Poor Glycemic Control
In diabetics, unpredictable digestion complicates insulin timing.
Understanding why Gastroparesis Causes Nausea is critical for preventing these complications.
Diagnosis of Gastroparesis
Doctors typically use several methods to confirm the condition:
- Gastric emptying study
- Upper endoscopy
- Imaging studies
- Blood tests
A gastric emptying study measures how long it takes food to leave the stomach. Delayed results confirm the diagnosis.
Treatment Strategies
Because Gastroparesis Causes Nausea due to delayed emptying, treatment focuses on improving stomach motility and controlling symptoms.
1. Dietary Modifications
Diet is the cornerstone of management.
Recommendations:
- Small, frequent meals
- Low-fat foods
- Low-fiber foods
- Soft or liquid meals
- Thorough chewing
Liquids empty faster than solids, which can significantly reduce Nausea After Eating.
- Medications
Several medications may help:
- Prokinetics (stimulate stomach movement)
- Antiemetics (reduce nausea)
- Acid reducers
These drugs aim to either improve motility or reduce nausea signals.
3. Blood Sugar Control
In diabetic patients, tight glucose management helps prevent nerve damage progression.
Stable blood sugar reduces nausea triggers.
4. Gastric Electrical Stimulation
In severe cases, a surgically implanted device delivers electrical pulses to stimulate stomach muscles.
This can reduce chronic nausea in some patients.
5. Feeding Tubes or IV Nutrition
For severe malnutrition, alternative feeding methods may be necessary.
Lifestyle Adjustments to Reduce Nausea After Eating
Beyond medical treatments, daily habits can significantly affect symptoms.
Eat Slowly
Rushing increases air swallowing and distension.
Sit Upright After Meals
Gravity helps move food downward.
Avoid Lying Down for 2 Hours
Lying flat can worsen nausea.
Gentle Walking
Light activity stimulates digestion.
Psychological Impact of Chronic Nausea
Persistent Nausea After Eating can take a mental toll. Anxiety around meals, fear of vomiting, and social withdrawal are common.
Chronic illness often leads to:
- Depression
- Stress
- Reduced quality of life
Addressing mental health is an important part of managing why Gastroparesis Causes Nausea.
Emerging Research
Researchers are exploring:
- New prokinetic drugs
- Microbiome therapies
- Neuromodulation techniques
- Regenerative nerve treatments
Understanding the precise mechanisms behind Gastroparesis Causes Nausea may lead to more targeted therapies in the future.
When to See a Doctor
Seek medical attention if you experience:
- Persistent Nausea After Eating
- Vomiting undigested food
- Unintentional weight loss
- Severe bloating
- Blood sugar instability
Early diagnosis improves symptom control.
Practical Meal Example for Managing Symptoms
Breakfast: Smooth yogurt with blended fruit
Snack: Low-fat soup
Lunch: Mashed potatoes with soft protein
Snack: Protein shake
Dinner: Steamed fish with well-cooked vegetables
Liquid and soft meals reduce stomach workload and help prevent Nausea After Eating.
Long-Term Outlook
Gastroparesis is often chronic but manageable. While symptoms fluctuate, many people achieve better control with consistent dietary adjustments and medical care.
Recognizing that Gastroparesis Causes Nausea because of delayed gastric emptying empowers patients to make informed decisions about food choices and treatment options.
Conclusion
Understanding why Gastroparesis Causes Nausea requires examining how the stomach normally empties and what happens when that process slows down. When food remains in the stomach too long, it stretches the stomach walls, disrupts normal electrical rhythms, increases fermentation, and stimulates powerful nausea signals.
This is why Nausea After Eating is such a defining and distressing symptom of gastroparesis.
Although the condition can significantly impact quality of life, effective management strategies exist. Through dietary modifications, medication, blood sugar control, and lifestyle adjustments, many individuals can reduce nausea and improve their daily functioning.
If you experience persistent nausea after meals, consult a healthcare professional. Early evaluation and proper treatment can prevent complications and help restore comfort around eating.
By understanding the mechanisms behind the condition, patients and caregivers can better navigate the challenges of gastroparesis and work toward improved digestive health.