Gastroparesis Treatment is a critical aspect of managing a chronic digestive disorder that significantly affects quality of life. Gastroparesis, sometimes called delayed gastric emptying, is a condition in which the stomach empties food into the small intestine more slowly than normal, without any physical blockage. The disorder can lead to persistent nausea, vomiting, abdominal pain, bloating, malnutrition, and unstable blood sugar levels.
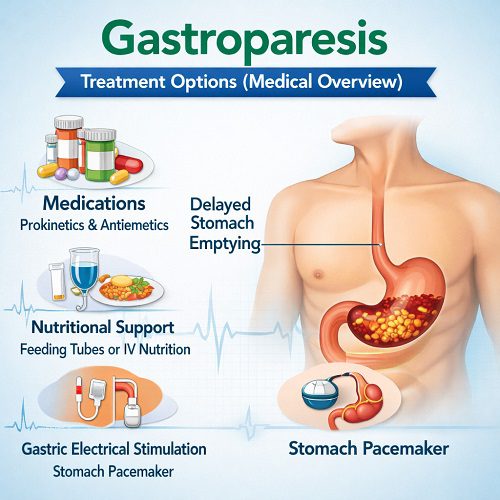
Effective Gastroparesis Treatment requires a comprehensive, individualized approach. It often involves dietary changes, medications, medical devices, and in severe cases, surgical interventions. Because the condition can vary widely in severity and cause, treatment strategies must be tailored to each patient’s needs.
This medical overview explores the available Gastroparesis Treatment options, including lifestyle interventions, pharmacologic therapies, procedural treatments, and emerging therapies.
Understanding Gastroparesis
Gastroparesis occurs when the stomach muscles fail to contract properly. Normally, coordinated muscle contractions move food from the stomach into the small intestine. In gastroparesis, this motility process is impaired.
Common causes include:
- Diabetes (especially long-standing or poorly controlled)
- Post-surgical nerve damage
- Certain medications (e.g., opioids, anticholinergics)
- Neurological disorders
- Idiopathic (unknown cause)
Symptoms often include:
- Chronic nausea
- Vomiting (sometimes of undigested food hours later)
- Early satiety
- Bloating
- Upper abdominal pain
- Weight loss
- Poor blood glucose control in diabetic patients
The primary goal of Gastroparesis Treatment is to relieve symptoms, improve gastric emptying, maintain nutrition, and manage underlying causes.
Goals of Gastroparesis Treatment
Effective Gastroparesis Treatment focuses on:
- Improving gastric emptying
- Reducing nausea and vomiting
- Maintaining adequate nutrition and hydration
- Stabilizing blood glucose (if diabetic)
- Preventing complications such as bezoars and malnutrition
Treatment plans often progress from conservative strategies to more advanced interventions depending on severity.
Dietary and Nutritional Management
Dietary modification is the foundation of Gastroparesis Treatment.
Small, Frequent Meals
Patients are typically advised to eat:
- 4–6 small meals daily
- Smaller portion sizes
- Soft or liquid foods
Smaller meals reduce the burden on delayed gastric emptying.
Low-Fat and Low-Fiber Diet
Fat slows gastric emptying and fiber can form indigestible masses (bezoars). Therefore:
- Low-fat foods are recommended
- High-fiber foods (raw vegetables, legumes, certain fruits) are limited
- Tough meats and fibrous foods are avoided
Liquid Nutrition
Liquids empty from the stomach more easily than solids. Nutritional shakes or soups are often better tolerated. In moderate to severe cases, patients may rely heavily on liquid nutrition.
Glycemic Control in Diabetic Patients
For individuals with diabetic gastroparesis, optimizing blood glucose levels is a critical component of Gastroparesis Treatment. Hyperglycemia itself slows gastric emptying, creating a vicious cycle.
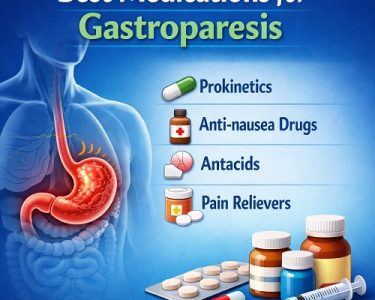
Pharmacologic Gastroparesis Treatment
Medications are commonly used when dietary changes alone are insufficient.
Prokinetic Agents
Prokinetic drugs stimulate stomach contractions and improve motility.
Metoclopramide
Metoclopramide is the only FDA-approved medication specifically for gastroparesis in the United States.
Mechanism:
- Dopamine receptor antagonist
- Enhances gastric motility
- Reduces nausea
Limitations:
- Risk of tardive dyskinesia with long-term use
- Generally recommended for short-term therapy
Because of potential neurological side effects, it must be used cautiously.
Erythromycin
Erythromycin acts as a motilin receptor agonist, stimulating gastric contractions.
Benefits:
- Effective short-term
- Often used in hospitalized patients
Drawbacks:
- Tachyphylaxis (diminishing effect over time)
- Gastrointestinal side effects
Antiemetics
These medications reduce nausea and vomiting but do not improve gastric emptying.
Commonly used agents include:
- Ondansetron
- Promethazine
They are supportive therapies within a broader Gastroparesis Treatment plan.
Device-Based and Procedural Gastroparesis Treatment
When medications and dietary measures fail, more advanced interventions may be considered.
Gastric Electrical Stimulation (GES)
Enterra Therapy System is an implantable device that delivers electrical pulses to the stomach.
Indications:
- Severe, medication-refractory gastroparesis
- Particularly helpful in diabetic patients
Benefits:
- Reduction in nausea and vomiting frequency
- Improved quality of life in select patients
Limitations:
- Requires surgical implantation
- Variable response rates
GES is not a cure but can significantly improve symptoms in appropriately selected individuals.
Endoscopic and Surgical Interventions
Gastric Peroral Endoscopic Myotomy (G-POEM)
G-POEM is a minimally invasive endoscopic procedure that cuts the pyloric muscle to facilitate gastric emptying.
Advantages:
- Less invasive than traditional surgery
- Promising outcomes in selected patients
Risks:
- Bleeding
- Perforation
- Infection
G-POEM is increasingly recognized as an important option in refractory Gastroparesis Treatment.
Pyloroplasty
Surgical pyloroplasty involves enlarging the pyloric opening to improve emptying.
It may be considered for:
- Severe cases
- Patients not responding to medications or GES
Feeding Tubes
In cases of severe malnutrition:
- Jejunostomy tubes may be placed for direct small intestinal feeding
- Venting gastrostomy tubes can relieve pressure and vomiting
Feeding tubes are typically reserved for advanced disease.
Emerging and Investigational Therapies
Research into Gastroparesis Treatment continues to evolve.
Ghrelin Agonists
Ghrelin stimulates appetite and gastric motility. Investigational drugs targeting ghrelin receptors show promise in improving emptying times.
Novel Prokinetics
New agents aim to improve gastric contractions without the neurological side effects associated with older drugs.
Stem Cell and Neuromodulation Research
Experimental studies are evaluating:
- Regeneration of enteric neurons
- Advanced neuromodulation techniques
While not yet standard care, these innovations may shape the future of Gastroparesis Treatment.
Managing Underlying Causes
A key principle of effective Gastroparesis Treatment is addressing underlying contributors.
Diabetes Management
Improving glycemic control:
- Reduces symptom severity
- Improves gastric emptying
- Prevents progression
Insulin regimens may need adjustment due to unpredictable absorption.
Medication Review
Certain drugs slow gastric emptying:
- Opioids
- Anticholinergics
- GLP-1 receptor agonists
Adjusting or discontinuing these medications can significantly improve symptoms.
Complications and Long-Term Management
Gastroparesis is often chronic. Long-term Gastroparesis Treatment focuses on:
- Monitoring nutritional status
- Preventing dehydration
- Avoiding hospitalizations
- Addressing psychological impacts
Bezoars
Poor gastric motility can cause bezoars (hardened food masses). These may require:
- Endoscopic removal
- Enzymatic dissolution
Malnutrition
Regular nutritional assessment is critical. Dietitians play a central role in comprehensive care.
Multidisciplinary Approach to Gastroparesis Treatment
Optimal care often involves:
- Gastroenterologists
- Endocrinologists (for diabetic patients)
- Dietitians
- Surgeons
- Pain specialists
- Mental health professionals
Because symptoms can be debilitating and affect daily function, psychological support may also improve outcomes.
Individualizing Gastroparesis Treatment
No single Gastroparesis Treatment works for everyone. Management depends on:
- Cause of gastroparesis
- Severity of symptoms
- Nutritional status
- Response to previous therapies
- Patient preferences
Mild cases may respond well to diet modification alone, while severe cases may require a combination of medications, device therapy, and procedural interventions.
Prognosis and Quality of Life
Gastroparesis can be unpredictable. Some patients experience fluctuating symptoms, while others develop progressive disease.
With appropriate Gastroparesis Treatment:
- Many patients achieve symptom improvement
- Hospitalizations may decrease
- Nutritional status can be maintained
- Quality of life can improve significantly
However, ongoing follow-up is essential, especially in diabetic patients where blood sugar control plays a central role.
Conclusion
Gastroparesis Treatment requires a comprehensive and individualized strategy. From dietary modification and medication to advanced device-based and surgical interventions, management options continue to expand. Early diagnosis and tailored therapy are crucial to preventing complications and maintaining nutritional health.
While there is currently no cure for gastroparesis, modern Gastroparesis Treatment approaches can significantly reduce symptoms, improve gastric emptying, and enhance overall quality of life. Continued research into novel prokinetics, neuromodulation, and regenerative therapies holds promise for more effective and safer treatments in the future.
Patients experiencing persistent nausea, vomiting, bloating, or unexplained digestive symptoms should seek evaluation from a qualified healthcare provider. Early intervention can dramatically improve long-term outcomes and help patients regain control over their digestive health.