Rectal prolapse is a medical condition in which the rectum, the final part of the large intestine, slips out of its normal anatomical position and protrudes through the anus. This can occur partially, affecting only the inner lining of the rectum (mucosal prolapse), or completely, where the full thickness of the rectal wall extends outside the body. The severity of rectal prolapse can vary widely: in some cases, it appears only during bowel movements and retracts on its own, while in more severe cases, the protrusion remains visible and can cause pain, bleeding, mucus discharge, and difficulty controlling bowel movements. The condition is often associated with weakened pelvic floor muscles, chronic constipation, or damage to the supportive structures of the pelvis.
Pregnancy adds unique challenges that can increase the risk of this condition. Hormonal changes during pregnancy cause ligaments and connective tissues to relax, while the growing uterus puts additional pressure on the pelvic floor and rectal walls. These factors can lead to the development or worsening of rectal prolapse in pregnancy, causing discomfort, visible protrusion, and in some cases, complications if not addressed early. Recognizing the symptoms and understanding the underlying causes is crucial for pregnant women to ensure timely management and reduce the risk of serious complications.
What is Rectal Prolapse?
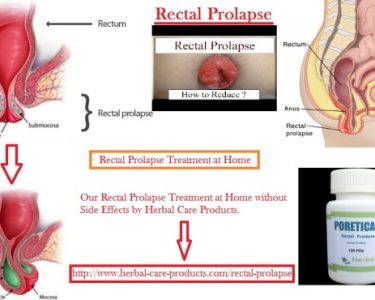
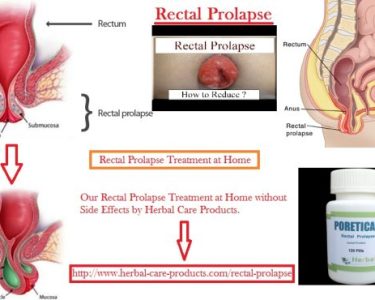
Rectal prolapse is a condition in which the rectum—the final segment of the large intestine—loses its normal anatomical support and protrudes through the anus. This displacement can occur in varying degrees. In a partial prolapse, only the mucosa, which is the inner lining of the rectum, slips out, while in a complete prolapse, the entire thickness of the rectal wall extends outside the body. In severe cases, the prolapsed rectum may remain permanently outside the anus, causing significant discomfort, bleeding, mucus discharge, and even fecal incontinence.
The condition arises when the muscles and ligaments that normally support the rectum weaken, making it unable to maintain its proper position. Factors such as chronic constipation, repeated straining during bowel movements, aging, connective tissue disorders, or prior pelvic injuries can contribute to this weakening.
During pregnancy, the risk of rectal prolapse can increase due to several physiological changes. The growing uterus exerts constant pressure on the pelvic floor, while pregnancy hormones like relaxin cause ligaments and connective tissues to become more flexible. This combination of mechanical pressure and tissue relaxation can stretch and weaken the muscles supporting the rectum, making it more likely for the rectum to slip out of place. Additionally, frequent constipation, which is common in pregnancy due to hormonal changes and reduced bowel motility, further increases the risk. As a result, women may experience new-onset rectal prolapse or a worsening of a pre-existing condition during pregnancy, especially in the later trimesters when the abdominal pressure is at its peak.
Causes of Rectal Prolapse:
Several factors contribute to the development of rectal prolapse, particularly in pregnant women:
Weak Pelvic Floor Muscles:
Pregnancy stretches the muscles and ligaments supporting the rectum, making it prone to prolapse.
Chronic Constipation:
Straining during bowel movements increases the risk.
Vaginal Delivery:
Multiple deliveries, especially with forceps or prolonged labor, can damage pelvic support structures.
Connective Tissue Disorders:
Some women may have underlying conditions that weaken tissues.
Age and Previous Surgeries:
Older pregnant women or those with prior pelvic surgeries are at higher risk. At times, rectal prolapse may occur suddenly or gradually worsen during the second or third trimester.
Symptoms of Rectal Prolapse
Recognizing rectal prolapse in pregnancy early is crucial. Symptoms vary depending on severity:
Visible Protrusion:
A noticeable bulge from the anus, especially during bowel movements.
Rectal Bleeding:
Mild bleeding may occur due to irritation of the protruded tissue.
Mucus Discharge:
The rectum may secrete mucus, causing discomfort.
Pain or Discomfort:
Some women experience anal or rectal pain, particularly when sitting.
Fecal Incontinence:
In severe cases, there may be difficulty controlling bowel movements.
Feeling of Incomplete Evacuation:
A sensation that bowel movements are incomplete or obstructed. Rectal bleeding inflammatory bowel disease can sometimes mimic these symptoms, so proper medical evaluation is essential to rule out other conditions.
Is Rectal Prolapse Common in Pregnancy?
Many women wonder, is rectal prolapse common in pregnancy? While it is relatively rare, the risk increases with certain factors such as:
- Multiple pregnancies
- Chronic constipation
- Vaginal trauma during delivery
- Weak pelvic floor muscles
Although not a common condition, awareness is important because even a mild prolapse can cause discomfort and lead to complications if ignored.
Is Rectal Prolapse Dangerous in Pregnancy?
The next question that arises is, is rectal prolapse dangerous in pregnancy?
In most cases, mild rectal prolapse does not pose a serious threat to the baby. However, severe prolapse can lead to:
- Strangulation of the prolapsed tissue
- Persistent bleeding and infection
- Difficulty in bowel movements
- Pain that interferes with daily activities and pregnancy comfort
Early detection and proper management are key to preventing these complications.
Rectal Prolapse in Late Pregnancy
Many cases of rectal prolapse occur during late pregnancy due to increased intra-abdominal pressure and the stretching of pelvic floor muscles. Women in their third trimester may notice:
- Worsening protrusion of the rectum
- Increased difficulty with bowel movements
- Greater anal discomfort, particularly while sitting or walking
It is essential to report these symptoms promptly to a healthcare provider, as timely intervention can prevent further complications.
Rectal Prolapse in Pregnancy Treatment
Rectal prolapse in pregnancy treatment primarily focuses on relieving symptoms and supporting the pelvic floor. Treatment strategies include:
Lifestyle Adjustments:
- Avoid straining during bowel movements
- Maintain a high-fiber diet and proper hydration
- Use stool softeners if recommended
Pelvic Floor Exercises:
Kegel exercises can strengthen the muscles supporting the rectum and reduce prolapse risk.
Supportive Devices:
Pessaries may be used to support pelvic organs temporarily in some cases.
Surgical Intervention:
Surgery is usually avoided during pregnancy unless absolutely necessary. Most women undergo corrective procedures after delivery. Natural remedies for rectal prolapse can also help improve comfort, though they should be used under the guidance of a healthcare professional. Similarly, some women explore herbal remedies for rectal prolapse as complementary therapy.
Risk Factors and Prevention
Preventing rectal prolapse involves proactive management of risk factors:
Preventing Constipation:
A diet rich in fiber, adequate fluid intake, and regular exercise can reduce strain.
Pelvic Floor Strengthening:
Consistent Kegel exercises before and during pregnancy help maintain muscle tone.
Avoid Heavy Lifting:
Reduces intra-abdominal pressure that may worsen prolapse.
Monitor Symptoms:
Early recognition of discomfort, bleeding, or protrusion allows timely intervention. Treatment of rectal prolapse symptoms is easier and more effective when addressed early.
When to Seek Medical Help
Immediate medical attention is recommended if a pregnant woman experiences:
- Persistent or severe rectal pain
- Visible protrusion that does not retract
- Significant bleeding
- Signs of infection such as fever or discharge
Prompt evaluation ensures both maternal and fetal safety.
Prognosis and Recovery
With timely intervention, most women recover well from rectal prolapse, especially postpartum. Strengthening pelvic muscles and following medical advice significantly reduces recurrence. Post-delivery, more definitive treatments, including surgical correction, can be considered if symptoms persist. Rectal prolapse symptoms and prolapsed bowel treatment strategies after delivery often lead to long-term relief.
Complementary and Natural Approaches
While medical supervision is essential, several complementary approaches may support recovery:
- Natural treatment for rectal prolapse through pelvic floor exercises
- Herbal and gentle remedies to soothe discomfort
- Lifestyle modifications such as avoiding straining and maintaining bowel regularity
Rectal prolapse mucosal prolapse may sometimes respond well to non-surgical interventions, particularly when detected early.
Conclusion
Rectal prolapse in pregnancy is a challenging but manageable condition. Early recognition of critical signs such as visible protrusion, pain, and bleeding is essential. Understanding the causes, risk factors, and available treatment options empowers women to take proactive measures for their health and comfort.
By incorporating lifestyle changes, pelvic floor exercises, and medical guidance, most women can prevent worsening symptoms and recover successfully postpartum. Awareness and timely intervention are key to minimizing discomfort and ensuring a safe pregnancy journey.
Natural Remedies for Rectal Prolapse at home can complement medical care, while professional treatment remains the cornerstone for severe cases. With proper care, rectal prolapse in pregnancy can be managed effectively, allowing women to focus on the joy of their pregnancy without unnecessary worry.