Living with bullous pemphigoid can be physically painful and emotionally draining, especially when you’re trying to manage daily activities like bathing or showering. If you’ve ever wondered, “can you shower with bullous pemphigoid?”, you’re not alone. Many patients worry that water, soap, or even gentle scrubbing might worsen their blisters or slow down healing.
In this comprehensive guide, we’ll explore how to shower safely when you have bullous pemphigoid, what precautions to take, and how to protect your skin barrier during flare-ups. You’ll also learn about the importance of gentle care, moisturizing, and maintaining hygiene without aggravating your symptoms.
Understanding Bullous Pemphigoid and Your Skin
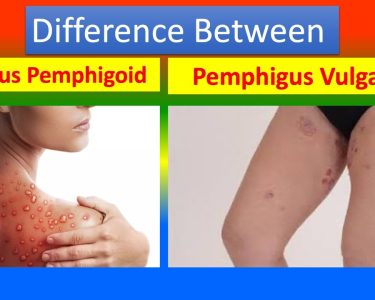
Before diving into the best showering practices, it’s important to understand what bullous pemphigoid actually is. This condition is an autoimmune blistering disorder that causes large, fluid-filled blisters to appear on the skin. It typically affects older adults, although it can occur in younger individuals as well.
When the immune system mistakenly attacks the layer of skin that connects the epidermis (top layer) to the dermis (lower layer), blisters and inflammation occur. The blisters are often itchy, tender, and prone to infection if not handled carefully.
Because the skin is already fragile, even gentle rubbing, heat, or harsh soaps can make the condition worse. This is why understanding how to shower safely is essential for comfort and skin protection.
Can You Shower with Bullous Pemphigoid?
Yes, you can shower with bullous pemphigoid, but it requires care and attention to detail. Showering is not harmful if done correctly — in fact, keeping the skin clean can help prevent infections that may develop from open blisters or lesions. However, how you shower and what you use on your skin make all the difference.
Dermatologists recommend using lukewarm water, gentle cleansers, and soft towels. Hot water can strip natural oils and worsen itching, while cold water may not effectively remove sweat or bacteria. The goal is to maintain hygiene without irritating the affected skin.
If your blisters are widespread or painful, you might consider shorter showers (5–10 minutes) and using minimal friction. You can also apply a light layer of emollient before stepping into the shower to provide a protective barrier.
Step-by-Step Guide to Safe Showering
Set the Right Water Temperature
Use lukewarm water. Hot water can increase inflammation and itching, while cold water can shock the skin and worsen sensitivity. Lukewarm temperatures help maintain comfort and prevent dehydration of the skin.
Choose Gentle Cleansers
Avoid antibacterial soaps, strong body washes, and products containing alcohol, fragrance, or sulfates. Instead, go for mild, pH-balanced cleansers designed for sensitive skin. Many patients find fragrance-free products or those with natural oils soothing.
Avoid Direct Water Pressure
When showering, avoid letting strong water pressure hit the blisters directly. A gentle flow or handheld showerhead can help you control where the water goes, reducing irritation and the risk of rupturing blisters.
Pat — Don’t Rub — Your Skin Dry
After showering, gently pat your skin dry with a soft cotton towel. Never rub, as friction can cause new blisters or tear existing ones. Using a separate towel for affected areas can help prevent secondary infections.
Apply Moisturizer Immediately
Within three minutes after your shower, apply a dermatologist-approved moisturizer or prescribed cream to lock in hydration. This helps strengthen the skin barrier and reduce itching.
Should You Shower Every Day?
Showering frequency depends on your skin’s condition and personal comfort. If your blisters are extensive or actively weeping, daily showers might be too harsh. In such cases, cleansing with a damp cloth or using gentle antiseptic wipes can help keep the skin clean without full immersion.
On the other hand, if your blisters are healing and not open, regular showers can support hygiene and comfort — just make sure to follow the steps mentioned above.
For patients undergoing treatment, always check with your dermatologist about specific bathing routines that complement your medical therapy.
Expert Advice on Soaps, Oils, and Bath Products
Choosing the right skincare products is critical when dealing with bullous pemphigoid. Dermatologists recommend avoiding soaps with harsh detergents, dyes, or perfumes. Instead, look for hypoallergenic or dermatologically tested cleansers.
Some people benefit from adding some natural remedies for bullous pemphigoid as like colloidal oatmeal, aloe vera gel, or coconut oil to their skincare routine. However, always test a small area first, as some natural products can still cause irritation in sensitive skin.
Moisturizers with ceramides or natural emollients like shea butter are excellent options to keep the skin hydrated after showering. You might also consider barrier creams or prescription ointments if your dermatologist recommends them.
Common Mistakes to Avoid When Showering
When managing bullous pemphigoid, small mistakes during showering can lead to big consequences. Avoid these common errors:
- Using hot water – It can increase inflammation and weaken the skin’s natural barrier.
- Scrubbing blisters – Even mild exfoliation can tear the fragile skin.
- Applying products on open blisters – Wait until lesions are healed before applying lotions or oils directly.
- Skipping moisturization – Dryness can worsen itching and lead to new blisters.
- Ignoring infected areas – Redness, swelling, or pus may indicate infection and need medical care.
Remember, your goal is to keep your skin clean and soothed — not stripped or inflamed.
Managing Blisters and Wounds Post-Shower
After showering, take a few extra minutes for proper wound care. If any blisters have burst, gently clean the area with sterile saline or mild antiseptic. Avoid hydrogen peroxide or alcohol-based solutions as they can delay healing.
Once the area is clean, apply prescribed ointments or steroid creams as directed by your doctor. Cover open blisters with non-stick gauze or breathable dressings to prevent infection.
This step is especially important because bullous pemphigoid blisters can take weeks to heal and often recur in the same areas if not protected.
When Bathing May Be Better Than Showering
In some cases, patients find that baths are more soothing than showers. A short soak in lukewarm water with mild emollients or oatmeal can calm itching and inflammation. However, always make sure that the water is clean, and avoid bubble baths or fragranced additives that can irritate the skin.
After bathing, gently pat dry and apply moisturizer immediately to prevent moisture loss. Baths can be an excellent alternative for those with severe lesions who cannot tolerate direct water flow.
Can You Shower with Bullous Pemphigoid During Flare-Ups?
During active flare-ups, showering should be done with extreme caution. If the blisters are open, painful, or oozing, limit water exposure and avoid any products except for those approved by your doctor.
You can still maintain hygiene by gently wiping unaffected areas with a damp cloth. Always follow your dermatologist’s advice, as certain topical medications or bandages may need to stay dry for effective healing.
Remember that bullous pemphigoid – autoimmune skin disorder causes the skin to be extra delicate, so patience and gentleness during flare-ups are essential for recovery.
The Role of a Healthy Routine in Recovery
Besides proper showering habits, maintaining a balanced skincare and lifestyle routine supports healing. Stress, harsh chemicals, and certain foods can sometimes worsen inflammation. A consistent routine that includes gentle cleansing, moisturizing, and a nutritious diet can make a huge difference in your comfort and healing speed.
Some patients explore treating bullous pemphigoid naturally alongside medical treatment, focusing on anti-inflammatory diets and gentle herbal remedies. While such approaches can support overall health, they should always be discussed with your healthcare provider before making any changes.
Supporting Young Adults with Bullous Pemphigoid
Though more common in older adults, bullous pemphigoid in young adults is increasingly recognized. Showering can be particularly distressing for younger individuals balancing work, studies, or social life. Education on proper hygiene, skincare, and emotional support plays a big role in managing this chronic condition.
Understanding that showers can still be safe — when done gently and with care — can help young adults maintain confidence and comfort in their daily lives.
Natural Approaches and Gentle Healing
For some individuals, complementary care with natural herbal treatment for bullous pemphigoid and symptoms may offer additional comfort. Natural oils like chamomile, calendula, or tea tree (diluted) are sometimes used to soothe the skin, but only under medical supervision.
The focus should always be on maintaining clean, hydrated skin and preventing infections. Natural methods can complement prescribed treatments but should never replace them entirely.
Dietary Considerations for Skin Protection
A balanced diet supports your immune system and overall skin health. Certain foods can trigger inflammation or allergic reactions, potentially worsening symptoms. For this reason, doctors often recommend paying attention to bullous pemphigoid natural treatment and some food avoid lists that may include highly processed foods, sugary items, or spicy meals.
Drinking enough water and eating antioxidant-rich foods like fruits, vegetables, and omega-3 fatty acids can help your skin repair naturally. Every patient is different, so always track what foods seem to affect your symptoms.
Exploring Natural Care and Lifestyle Changes
Some individuals find comfort in exploring bullous pemphigoid natural treatment strategies in addition to prescribed medications. These may include using hypoallergenic skincare products, maintaining stress management routines, and incorporating gentle exercise or meditation.
While natural approaches can support healing, they should always be balanced with professional medical care to avoid complications or delayed healing.
Key Takeaways: Showering Safely with Bullous Pemphigoid
If you’re still asking “can you shower with bullous pemphigoid?”, the answer is yes — with care and mindfulness. Here’s a quick summary of the main points:
- Use lukewarm water and gentle cleansers only.
- Pat dry, never rub your skin.
- Moisturize immediately after showering.
- Avoid direct water pressure on blisters.
- Keep showers short and soothing (5–10 minutes).
- Consult your dermatologist about specific products or routines.
Taking a shower shouldn’t be painful or risky. With the right precautions, it can actually help keep your skin clean, hydrated, and more comfortable during your recovery journey.
Final Thoughts
Living with bullous pemphigoid can be challenging, but understanding your skin and how to care for it makes all the difference. Showering, though seemingly simple, becomes an important part of your healing routine when done with awareness and gentleness.
By adopting the right bathing practices and using dermatologist-approved products, you can protect your skin barrier, reduce discomfort, and prevent further complications.
Remember: You can shower with bullous pemphigoid safely — it’s all about the right balance of care, comfort, and consistency.