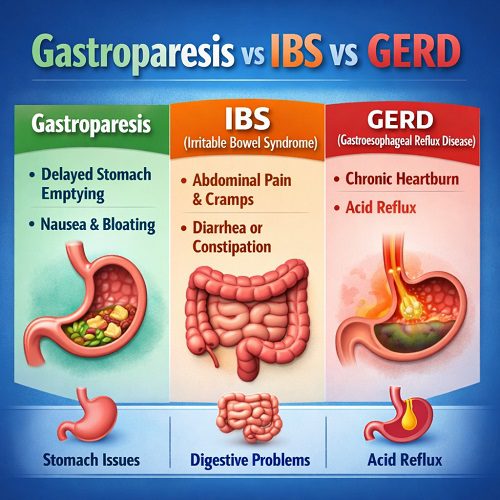
Digestive problems are among the most common health complaints worldwide. Symptoms like bloating, abdominal pain, nausea, heartburn, and irregular bowel movements can significantly affect daily life. Three conditions that are often confused due to overlapping symptoms are gastroparesis, irritable bowel syndrome (IBS), and gastroesophageal reflux disease (GERD). While they may share certain features, they are fundamentally different disorders affecting different parts of the digestive system.
Understanding the distinctions between gastroparesis, IBS, and GERD is essential for accurate diagnosis, effective treatment, and improved quality of life. This article explores each condition in detail, highlighting their causes, symptoms, diagnostic methods, and management strategies.
Overview of the Digestive System
To understand how these conditions differ, it helps to briefly review how the digestive system works. Food travels from the mouth through the esophagus into the stomach. The stomach breaks food down before passing it into the small intestine for nutrient absorption. The remaining waste then moves through the large intestine (colon) and is eventually eliminated.
- GERD primarily affects the esophagus.
- Gastroparesis affects the stomach.
- IBS mainly involves the large intestine.
Though they occur in different regions, the symptoms can overlap, leading to confusion and misdiagnosis.
What Is Gastroparesis?
Gastroparesis, also known as delayed gastric emptying, is a condition in which the stomach empties food into the small intestine more slowly than normal. Importantly, this delay occurs without a physical blockage.
Causes of Gastroparesis
The most common cause is diabetes. High blood sugar levels can damage the vagus nerve, which controls stomach muscles. When this nerve does not function properly, stomach muscles cannot contract effectively.
Other causes include:
- Post-surgical nerve damage
- Viral infections
- Certain medications (such as opioids and some antidepressants)
- Neurological disorders
- Idiopathic (unknown cause)
Symptoms of Gastroparesis
Common symptoms include:
- Nausea
- Vomiting (often of undigested food)
- Early satiety (feeling full quickly)
- Bloating
- Upper abdominal pain
- Loss of appetite
- Unintended weight loss
Symptoms often worsen after eating, especially large or high-fat meals.
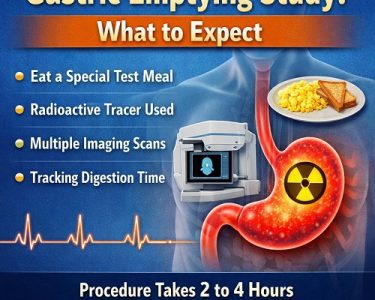
Diagnosis
Doctors typically use:
- Gastric emptying studies
- Upper endoscopy
- Imaging tests to rule out obstruction
Treatment
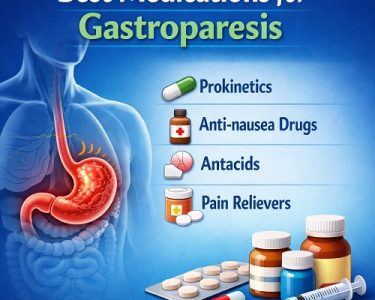
Treatment focuses on symptom management and improving gastric emptying:
- Dietary changes (small, frequent meals; low-fat and low-fiber foods)
- Blood sugar control (in diabetic patients)
- Prokinetic medications to stimulate stomach contractions
- Antiemetics to control nausea
- In severe cases, feeding tubes or gastric electrical stimulation
Gastroparesis can be chronic and difficult to manage, but many patients find relief through lifestyle adjustments and medical therapy.
What Is IBS (Irritable Bowel Syndrome)?
Irritable bowel syndrome is a functional gastrointestinal disorder affecting the large intestine. Unlike inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis, IBS does not cause visible inflammation or structural damage.
Types of IBS
IBS is categorized based on bowel habits:
- IBS-D (diarrhea-predominant)
- IBS-C (constipation-predominant)
- IBS-M (mixed)
- IBS-U (unclassified)
Causes of IBS
The exact cause is unknown, but contributing factors include:
- Abnormal gut motility
- Increased sensitivity to pain in the intestines
- Gut-brain axis dysfunction
- Stress and anxiety
- Changes in gut microbiota
- Previous gastrointestinal infections
Symptoms of IBS
Common symptoms include:
- Abdominal pain or cramping
- Bloating
- Gas
- Diarrhea, constipation, or alternating between both
- Mucus in stool
- Relief of pain after bowel movement
Symptoms are often triggered by stress or certain foods.
Diagnosis
There is no single test for IBS. Doctors use:
- Rome IV diagnostic criteria
- Symptom evaluation
- Tests to rule out other conditions (e.g., celiac disease, inflammatory bowel disease)
Treatment
Management typically includes:
- Dietary modifications (such as low-FODMAP diet)
- Increased fiber (for IBS-C)
- Antidiarrheal medications (for IBS-D)
- Antispasmodics
- Probiotics
- Stress management and cognitive behavioral therapy
IBS is chronic but manageable with the right combination of treatments.
What Is GERD (Gastroesophageal Reflux Disease)?
GERD is a chronic form of acid reflux. It occurs when stomach acid frequently flows back into the esophagus due to a weakened lower esophageal sphincter (LES).
Over time, repeated acid exposure can irritate the esophageal lining.
Causes of GERD
Common causes include:
- Weak or relaxed LES
- Hiatal hernia
- Obesity
- Pregnancy
- Smoking
- Certain foods (spicy, fatty, acidic)
- Large meals or lying down after eating
Symptoms of GERD
Typical symptoms include:
- Heartburn (burning sensation in chest)
- Acid regurgitation
- Chest pain
- Chronic cough
- Hoarseness
- Difficulty swallowing
- Sour taste in mouth
Symptoms often worsen after meals or when lying down.
Diagnosis
Doctors may use:
- Clinical symptom evaluation
- Upper endoscopy
- Esophageal pH monitoring
- Esophageal manometry
Treatment
Treatment options include:
- Lifestyle changes (weight loss, elevating head during sleep)
- Avoiding trigger foods
- Proton pump inhibitors (PPIs)
- H2 receptor blockers
- Antacids
- Surgery (such as fundoplication) in severe cases
Untreated GERD can lead to complications such as esophagitis or Barrett’s esophagus.
Key Differences Between Gastroparesis, IBS, and GERD
Feature | Gastroparesis | IBS | GERD |
| Affected Area | Stomach | Large intestine | Esophagus |
| Main Problem | Delayed stomach emptying | Altered bowel function | Acid reflux |
| Nausea/Vomiting | Common | Rare | Rare |
| Heartburn | Uncommon | Uncommon | Common |
| Bowel Changes | Usually normal | Core symptom | Usually normal |
| Early Fullness | Common | Sometimes | Sometimes |
| Structural Damage | No blockage | No visible damage | Possible esophageal damage |
Overlapping Symptoms and Misdiagnosis
Some symptoms overlap:
- Bloating occurs in all three.
- Abdominal discomfort can occur in both IBS and gastroparesis.
- Nausea can appear in GERD and gastroparesis.
- Upper abdominal pain may be seen in GERD and gastroparesis.
Because of this overlap, patients are sometimes initially misdiagnosed. For example, someone with chronic nausea and bloating may be labeled as having IBS when the real issue is delayed gastric emptying.
Accurate diagnosis requires careful history-taking and, when necessary, targeted testing.
Can Someone Have More Than One Condition?
Yes. It is possible for someone to have GERD and IBS simultaneously. In fact, research suggests that functional gastrointestinal disorders often overlap. A person with diabetes could develop gastroparesis and also experience GERD symptoms due to delayed stomach emptying increasing reflux risk.
This overlap makes comprehensive evaluation essential.
Lifestyle Factors and Dietary Considerations
Although each condition has distinct mechanisms, lifestyle changes benefit all three:
Common Helpful Strategies
- Eating smaller meals
- Avoiding large, fatty meals
- Staying upright after eating
- Managing stress
- Maintaining a healthy weight
Condition-Specific Diet Tips
Gastroparesis:
- Low-fat, low-fiber foods
- Soft or liquid meals
- Avoid carbonated drinks
IBS:
- Low-FODMAP diet
- Gradual fiber increase
- Identifying trigger foods
GERD:
- Avoid acidic, spicy, and fatty foods
- Limit caffeine and alcohol
- Avoid eating before bedtime
Personalized dietary adjustments are often necessary.
Psychological Impact and the Gut-Brain Connection
The digestive system is closely linked to the nervous system. Anxiety, depression, and chronic stress can worsen IBS and GERD symptoms. In gastroparesis, chronic nausea and vomiting may lead to social isolation and reduced quality of life.
Addressing mental health through therapy, relaxation techniques, or medication can significantly improve symptom control.
When to See a Doctor
Seek medical attention if you experience:
- Persistent vomiting
- Unintentional weight loss
- Difficulty swallowing
- Blood in stool or vomit
- Severe abdominal pain
- Chest pain
These could indicate complications or other serious conditions.
Conclusion
Gastroparesis, IBS, and GERD are distinct gastrointestinal disorders that affect different parts of the digestive tract but may share overlapping symptoms.
- Gastroparesis involves delayed stomach emptying and often presents with nausea and early fullness.
- IBS affects bowel habits and causes abdominal pain related to changes in stool.
- GERD results from acid reflux and primarily causes heartburn and regurgitation.
Accurate diagnosis is crucial because treatments differ significantly. While lifestyle and dietary modifications form the foundation of management for all three, medications and specific interventions vary depending on the condition.
If you experience persistent digestive symptoms, consult a healthcare professional for proper evaluation. With the right diagnosis and tailored treatment plan, most individuals can effectively manage symptoms and maintain a good quality of life.
Understanding the differences between gastroparesis, IBS, and GERD empowers patients to advocate for appropriate care and make informed decisions about their digestive health.