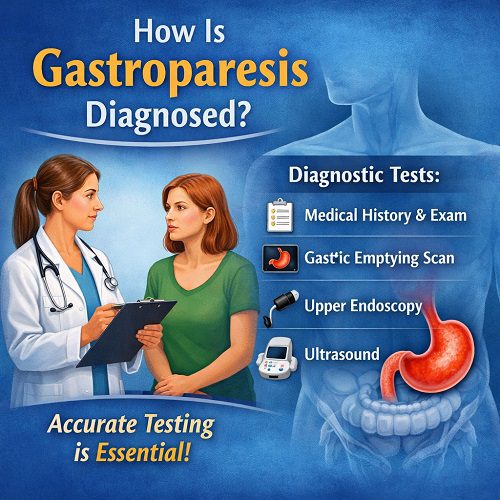
Understanding how Gastroparesis Diagnosed procedures work is essential for anyone experiencing persistent digestive symptoms such as nausea, vomiting, bloating, or early fullness. Gastroparesis is a chronic condition that affects the stomach’s ability to empty food properly. Because its symptoms overlap with many other gastrointestinal disorders, obtaining an accurate diagnosis requires a structured and thorough medical approach.
This article explains in detail how gastroparesis is diagnosed, what tests are involved, and what patients can expect during the evaluation process.
What Is Gastroparesis?
Gastroparesis is a digestive disorder in which the stomach empties more slowly than normal, without any physical blockage. The word itself literally means “stomach paralysis.” In healthy digestion, the stomach muscles contract to push food into the small intestine. In gastroparesis, these contractions are weak, irregular, or absent.
The condition is commonly associated with:
- Long-standing diabetes
- Nerve damage (particularly to the vagus nerve)
- Certain medications
- Autoimmune conditions
- Surgical complications
However, in many cases, the cause remains unknown (idiopathic gastroparesis).
Why Proper Diagnosis Is Important
The process of Gastroparesis Diagnosed correctly is crucial for several reasons:
- Symptoms mimic other digestive disorders such as acid reflux or irritable bowel syndrome.
- Treatment depends on confirming delayed gastric emptying.
- Misdiagnosis can lead to ineffective or harmful treatments.
- Complications such as malnutrition, dehydration, and unstable blood sugar can worsen without proper care.
Because there is no single symptom that confirms gastroparesis, diagnosis requires a combination of medical history, physical examination, and specialized testing.
Step 1: Medical History and Symptom Evaluation
The first step in how Gastroparesis Diagnosed procedures begin is a detailed discussion between the patient and healthcare provider.
Common Symptoms Reviewed
- Persistent nausea
- Vomiting undigested food hours after eating
- Feeling full quickly (early satiety)
- Bloating
- Abdominal discomfort
- Unexplained weight loss
- Poor appetite
- Blood sugar fluctuations (especially in diabetic patients)
The doctor will ask:
- When symptoms started
- How often they occur
- Whether symptoms worsen after meals
- Medication history
- Diabetes history
- Previous abdominal surgeries
This information helps determine whether delayed gastric emptying is likely.
Step 2: Physical Examination
Although a physical exam alone cannot confirm gastroparesis, it helps rule out other conditions.
During the exam, the doctor may:
- Check for abdominal tenderness
- Listen for abnormal bowel sounds
- Assess signs of dehydration
- Evaluate nutritional status
- Look for signs of systemic illness
If warning signs such as severe pain or bleeding are present, additional emergency testing may be ordered.
Step 3: Ruling Out Mechanical Obstruction
Before confirming Gastroparesis Diagnosed, physicians must ensure that symptoms are not caused by a physical blockage in the stomach or small intestine.
Upper Endoscopy
Upper endoscopy is commonly used to examine the esophagus, stomach, and upper small intestine.
During this procedure:
- A thin, flexible tube with a camera is inserted through the mouth.
- The doctor looks for ulcers, tumors, strictures, or inflammation.
- Biopsies may be taken if needed.
If food remains in the stomach after fasting, this may suggest delayed emptying, but further testing is still required.
Imaging Studies
Doctors may also order:
- Abdominal ultrasound
- CT scan
- Barium X-ray study
These tests help exclude structural abnormalities before confirming gastroparesis.
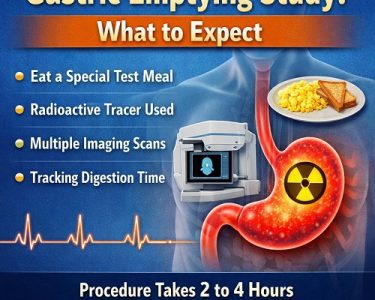
Step 4: Gastric Emptying Study (Gold Standard Test)
The most important test in how Gastroparesis Diagnosed is confirmed is the gastric emptying study.
Gastric Emptying Scintigraphy
Gastric emptying scintigraphy is considered the gold standard diagnostic test.
How It Works:
- The patient eats a small meal (often eggs or oatmeal) containing a tiny amount of radioactive material.
- A scanner tracks how quickly the food leaves the stomach.
- Images are taken over 2–4 hours.
What Results Mean:
- Normal: Most food empties within 4 hours.
- Gastroparesis: More than 10% of food remains in the stomach after 4 hours.
This test directly measures delayed gastric emptying and confirms the diagnosis.
Step 5: Breath Tests
Another method used in how Gastroparesis Diagnosed is evaluated involves non-radioactive breath testing.
Gastric Emptying Breath Test
Gastric emptying breath test measures digestion using a special meal containing a harmless substance absorbed in the intestine and detected in the breath.
The patient:
- Eats the test meal.
- Breath samples are collected over several hours.
- The rate of digestion is calculated.
While not as widely available as scintigraphy, it provides a safe and radiation-free alternative.
Step 6: Wireless Motility Capsule
Some patients undergo testing with a small electronic capsule.
SmartPill (Wireless Motility Capsule)
SmartPill is swallowed like a vitamin.
It measures:
- Stomach pH
- Pressure
- Temperature
- Transit time through the digestive tract
Data is transmitted to a wearable receiver. This test helps determine whether delayed emptying is isolated to the stomach or affects the entire digestive tract.
Step 7: Blood Tests and Lab Work
Although blood tests cannot directly diagnose gastroparesis, they help identify contributing factors.
Doctors may check:
- Blood glucose levels
- Thyroid function
- Electrolytes
- Kidney function
- Nutritional markers
- Vitamin deficiencies
For diabetic patients, poorly controlled blood sugar is a common contributor to delayed gastric emptying.
Special Considerations in Diabetic Patients
In people with diabetes, Gastroparesis Diagnosed procedures may require additional monitoring.
High blood sugar can:
- Slow stomach emptying
- Damage the vagus nerve
- Worsen nausea and vomiting
Doctors often recommend:
- Tight glucose control before testing
- Adjusting insulin timing
- Coordinating care between gastroenterologists and endocrinologists
Differential Diagnosis: Conditions That Mimic Gastroparesis
Several disorders produce similar symptoms, which is why thorough testing is essential.
These include:
- Gastroesophageal reflux disease (GERD)
- Peptic ulcer disease
- Functional dyspepsia
- Irritable bowel syndrome
- Intestinal obstruction
- Pancreatic disease
Proper testing ensures the diagnosis is accurate and prevents unnecessary treatment.
When to See a Doctor
You should seek medical evaluation if you experience:
- Persistent vomiting
- Inability to keep food down
- Unintentional weight loss
- Severe bloating
- Blood sugar instability
- Signs of dehydration
Early diagnosis improves outcomes and reduces complications.
What Happens After Gastroparesis Is Diagnosed?
Once Gastroparesis Diagnosed is confirmed, treatment planning begins.
Management may include:
- Dietary modifications (small, frequent meals)
- Low-fat, low-fiber diet
- Medications to stimulate stomach contractions
- Antiemetic drugs for nausea
- Blood sugar management
- Feeding tubes in severe cases
- Gastric electrical stimulation therapy
Treatment is individualized based on severity and underlying cause.
How Long Does Diagnosis Take?
The timeline for how Gastroparesis Diagnosed varies depending on:
- Symptom severity
- Test availability
- Underlying medical conditions
- Specialist referrals
For some patients, diagnosis may take weeks or months because symptoms overlap with other disorders.
Emotional and Psychological Impact
Living with unexplained digestive symptoms can be stressful. Many patients feel frustrated during the diagnostic process. Proper evaluation not only confirms the condition but also provides relief in understanding what is happening.
Support from healthcare providers, nutritionists, and mental health professionals can improve quality of life.
Advances in Diagnostic Research
Ongoing research continues to refine how Gastroparesis Diagnosed more accurately and efficiently.
Emerging areas include:
- Improved motility testing technology
- Biomarker research
- Advanced imaging methods
- Artificial intelligence interpretation of motility data
These advancements may lead to earlier detection and more personalized treatment approaches.
Preparing for Diagnostic Testing
If you are scheduled for testing, doctors may advise:
- Fasting before the procedure
- Avoiding certain medications
- Controlling blood sugar
- Stopping narcotic pain medications
- Avoiding smoking before testing
Following preparation instructions ensures accurate results.
Common Myths About Gastroparesis Diagnosis
Myth 1: Symptoms Alone Confirm Diagnosis
False. Objective testing is required.
Myth 2: Endoscopy Alone Diagnoses Gastroparesis
False. It rules out obstruction but does not measure emptying time.
Myth 3: It Only Affects Diabetics
False. Many cases are idiopathic.
Summary: How Is Gastroparesis Diagnosed?
To summarize, Gastroparesis Diagnosed involves a systematic approach:
- Detailed symptom review
- Physical examination
- Ruling out mechanical obstruction
- Confirming delayed gastric emptying with scintigraphy
- Using alternative tests if necessary
- Evaluating underlying causes
The gold standard remains gastric emptying scintigraphy, but other supportive tests help refine the diagnosis.
Early and accurate diagnosis allows patients to receive appropriate dietary guidance, medications, and lifestyle modifications that can significantly improve daily functioning.
Final Thoughts
Understanding how Gastroparesis Diagnosed empowers patients to advocate for proper testing and care. Because symptoms can be confusing and overlap with other digestive conditions, persistence and thorough evaluation are essential.
If you suspect gastroparesis, consult a healthcare provider and discuss appropriate diagnostic testing. With proper evaluation and management, many people learn to control symptoms and improve their quality of life.
Accurate diagnosis is the first step toward effective treatment and long-term digestive health.