Digestive discomfort is common, but when symptoms become persistent, progressive, and debilitating, they may signal a more serious underlying condition. One such disorder is gastroparesis — a chronic condition that affects the stomach’s ability to empty properly. While mild cases may cause intermittent discomfort, severe gastroparesis can significantly impact nutrition, daily functioning, and overall quality of life.
Understanding Gastroparesis Symptoms is essential for early recognition, timely diagnosis, and proper management. In this in-depth guide, we will explore what gastroparesis is, why it happens, the full spectrum of mild to severe symptoms, warning signs that require urgent medical attention, complications, diagnostic approaches, and available treatment strategies.
What Is Gastroparesis?
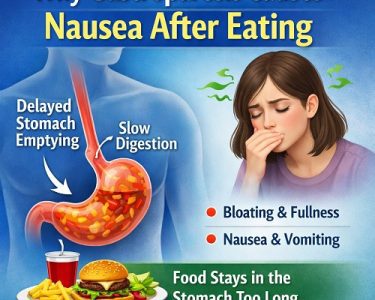
Gastroparesis is a condition in which the stomach empties food into the small intestine more slowly than normal, without a physical blockage. The word “gastro” refers to the stomach, and “paresis” means partial paralysis.
In healthy digestion:
- Food enters the stomach.
- The stomach muscles contract rhythmically.
- Food is broken down and gradually released into the small intestine.
In gastroparesis:
- Stomach muscle contractions are weak or uncoordinated.
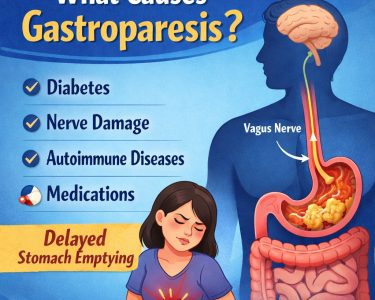
- The vagus nerve, which controls stomach movement, may be damaged.
- Food remains in the stomach for prolonged periods.
This delayed emptying leads to a range of digestive problems — and in severe cases, serious medical complications.
Why Gastroparesis Happens
Several underlying factors can damage the nerves or muscles responsible for gastric motility.
1. Diabetes
Long-standing diabetes is one of the most common causes. High blood sugar damages nerves, including the vagus nerve.
Diabetes mellitus is strongly linked to gastroparesis, especially when blood sugar levels are poorly controlled.
2. Post-Surgical Complications
Surgeries involving the stomach or esophagus can disrupt nerve pathways.
3. Viral Infections
Some viral illnesses temporarily inflame or damage stomach nerves.
4. Autoimmune Disorders
The immune system may mistakenly attack nerve tissue.
5. Medications
Certain drugs slow gastric emptying, including:
- Opioids
- Some antidepressants
- Anticholinergic medications
6. Idiopathic Cases
In many individuals, no clear cause is found. This is known as idiopathic gastroparesis.
Understanding Gastroparesis Symptoms
The severity of Gastroparesis Symptoms can vary widely. Some people experience mild nausea and fullness, while others struggle with debilitating vomiting and malnutrition.
Below is a detailed breakdown of symptoms — from early signs to severe complications.
Early Gastroparesis Symptoms
In the initial stages, symptoms may be subtle and intermittent.
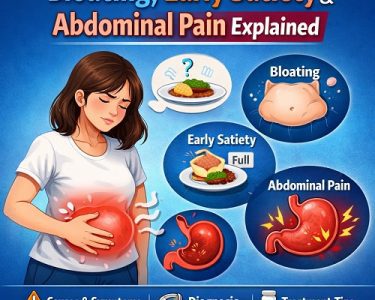
1. Early Satiety
Feeling full after eating only a small amount of food.
2. Post-Meal Bloating
A sensation of abdominal swelling and tightness.
3. Mild Nausea
Often worse after eating.
4. Upper Abdominal Discomfort
A dull ache or pressure in the upper stomach area.
5. Reduced Appetite
Food may feel unappealing due to persistent fullness.
These early Gastroparesis Symptoms are often mistaken for indigestion or stress-related digestive issues.
Moderate Gastroparesis Symptoms
As the condition progresses, symptoms become more persistent and disruptive.
1. Frequent Nausea
Daily nausea that interferes with eating.
2. Vomiting Undigested Food
Food eaten hours earlier may be vomited intact.
3. Acid Reflux
Delayed emptying increases pressure in the stomach.
Gastroesophageal Reflux Disease commonly overlaps with gastroparesis.
4. Abdominal Pain
Cramping or burning discomfort in the upper abdomen.
5. Fluctuating Blood Sugar
Particularly in people with Diabetes mellitus, delayed digestion causes unpredictable glucose absorption.
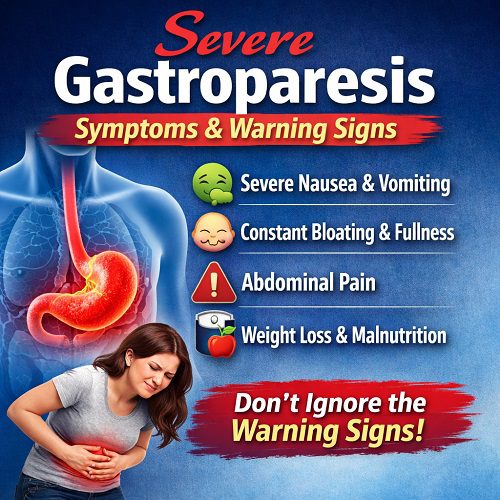
Severe Gastroparesis Symptoms
Severe cases can become medically dangerous. Recognizing warning signs is critical.
1. Persistent Vomiting
Repeated vomiting can lead to:
- Dehydration
- Electrolyte imbalance
- Weight loss
- Hospitalization
2. Severe Malnutrition
When food intake is chronically limited, the body lacks essential nutrients.
Symptoms include:
- Fatigue
- Hair thinning
- Weakness
- Muscle loss
3. Significant Weight Loss
Unintentional weight loss is a red flag.
4. Bezoar Formation
Undigested food can harden into a mass called a bezoar. This can block the stomach outlet and worsen symptoms.
5. Dehydration
Vomiting and poor intake reduce fluid levels, causing:
- Dizziness
- Dry mouth
- Low blood pressure
6. Severe Abdominal Pain
Pain may become sharp and persistent, requiring evaluation.
Warning Signs That Require Immediate Medical Attention
Seek urgent care if you experience:
- Vomiting blood
- Black or tarry stools
- Inability to keep fluids down
- Severe dehydration
- Confusion
- Rapid heart rate
- Severe weakness
These symptoms may signal complications such as obstruction or electrolyte imbalance.
The Emotional and Psychological Impact
Chronic digestive disorders affect more than just the stomach.
Living with severe Gastroparesis Symptoms can lead to:
- Anxiety about eating
- Fear of vomiting
- Social isolation
- Depression
- Nutritional stress
The unpredictability of flare-ups makes planning meals and social events difficult.
Complications of Severe Gastroparesis
Without proper management, gastroparesis can lead to serious complications.
1. Malnutrition
Insufficient calorie intake weakens the immune system.
2. Blood Sugar Instability
For people with Diabetes mellitus, delayed digestion makes insulin timing difficult.
3. Esophagitis
Repeated vomiting irritates the esophagus.
4. Bezoars
Solid masses of undigested food can block the stomach.
5. Hospitalization
Severe dehydration or electrolyte imbalance may require IV fluids.
How Gastroparesis Is Diagnosed
Diagnosis begins with symptom review and ruling out mechanical obstruction.
1. Gastric Emptying Study
The gold standard test measures how quickly food leaves the stomach.
2. Upper Endoscopy
Examines the stomach lining for ulcers or blockages.
3. Imaging Tests
CT scans or ultrasounds rule out structural problems.
4. Blood Tests
Check for:
- Electrolyte imbalances
- Nutritional deficiencies
- Blood sugar levels
Treatment Options for Gastroparesis Symptoms
There is no cure for gastroparesis, but treatments can significantly reduce symptoms.
Dietary Modifications
Diet plays a crucial role in symptom management.
Recommendations include:
- Small, frequent meals
- Low-fat foods
- Low-fiber foods
- Soft or liquid meals
- Thorough chewing
Liquids empty faster than solids and are often better tolerated.
Blood Sugar Control
For individuals with Diabetes mellitus, tight glucose management is essential.
Medications
Doctors may prescribe:
- Prokinetics (stimulate stomach movement)
- Antiemetics (reduce nausea)
- Acid suppressants
- Pain management medications
Gastric Electrical Stimulation
In severe cases, a device may be surgically implanted to stimulate stomach contractions.
Feeding Tubes
When oral intake is insufficient, nutrition may be delivered through:
- Jejunostomy tube
- Temporary IV nutrition
Lifestyle Adjustments for Severe Gastroparesis Symptoms
Managing daily life with gastroparesis requires strategy.
Helpful Habits:
- Sit upright after eating
- Avoid lying down for 2–3 hours post-meal
- Drink fluids between meals
- Avoid carbonated beverages
- Gentle walking after meals
Risk Factors for Severe Disease Progression
Some individuals are more likely to develop severe symptoms:
- Long-standing diabetes
- Poor blood sugar control
- Connective tissue disorders
- Previous stomach surgery
- Chronic opioid use
Gastroparesis vs Other Digestive Disorders
Symptoms often overlap with:
- Irritable Bowel Syndrome
- Gastroesophageal Reflux Disease
- Peptic ulcer disease
- Functional dyspepsia
Proper testing ensures accurate diagnosis.
Long-Term Outlook
Gastroparesis is typically chronic. However:
- Symptoms may fluctuate.
- Some post-viral cases improve.
- Proper management reduces complications.
Early recognition of worsening Gastroparesis Symptoms improves outcomes.
When to See a Doctor
Consult a healthcare provider if you experience:
- Persistent nausea
- Frequent vomiting
- Early fullness
- Unexplained weight loss
- Unstable blood sugars
- Chronic abdominal pain
Early intervention prevents progression.
Living with Severe Gastroparesis
While severe cases can feel overwhelming, many individuals learn to manage symptoms effectively through:
- Structured meal planning
- Regular medical monitoring
- Emotional support
- Nutritional counseling
- Medication adherence
Support groups and mental health care can significantly improve quality of life.
Final Thoughts
Severe gastroparesis is more than occasional indigestion — it is a complex disorder that can profoundly affect health and daily living. Recognizing Gastroparesis Symptoms early allows for timely diagnosis, treatment, and prevention of complications.
Persistent nausea, vomiting, early fullness, and abdominal pain should never be ignored — especially if accompanied by weight loss or dehydration.
If you suspect gastroparesis, consult a healthcare professional. With proper management, many people can regain stability, improve nutrition, and live fuller lives despite the challenges.
Your digestive health matters — and understanding the warning signs is the first step toward taking control.