Gastroparesis is a challenging and often misunderstood digestive disorder that affects the stomach’s ability to empty food at a normal rate. Instead of moving smoothly into the small intestine, food may sit in the stomach much longer than it should, leading to symptoms like nausea, vomiting, early fullness, and bloating. While many people associate gastroparesis primarily with weight loss, the reality is far more complex. A significant number of patients actually struggle with the opposite issue: weight gain and gastroparesis. This can be especially confusing and emotionally overwhelming, as it contradicts the common belief that delayed stomach emptying always leads to weight loss.
For many individuals, this unexpected weight gain brings frustration and anxiety, particularly when they are already dealing with uncomfortable digestive symptoms. In their search for answers or relief, some explore various supportive options—such as discover the top natural supplements for gastroparesis relief—hoping to manage their symptoms more effectively. While supplements and medications may offer some improvement, understanding the condition itself remains the most important first step toward regaining control.
This comprehensive guide provides a clear and detailed look at gastroparesis, breaking down what it is, why it occurs, and how it affects the body. It also explains why weight gain and gastroparesis often go hand in hand, helping readers understand the underlying mechanisms that contribute to unexpected weight changes. By gaining this foundational knowledge, patients and caregivers can approach their health with greater clarity and confidence.
Understanding Gastroparesis: What Is This Condition?
Gastroparesis is a chronic condition in which the stomach muscles weaken or stop working properly. Normally, the stomach contracts to push food into the small intestine. However, in gastroparesis, these contractions slow down significantly or become irregular, causing delayed gastric emptying.
Why Does This Happen?
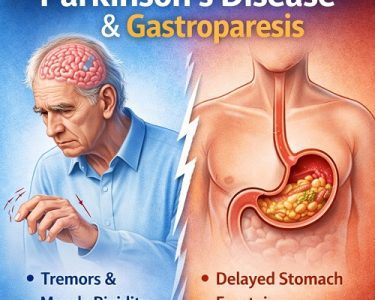
In a healthy digestive system, the vagus nerve controls stomach muscle movement. When this nerve becomes damaged, the communication between your brain and digestive organs becomes disrupted. As a result, food remains in the stomach for too long, leading to uncomfortable and sometimes severe symptoms.
Gastroparesis is not a rare condition. Millions of people live with it, but many remain undiagnosed because the symptoms mimic other digestive issues like acid reflux, ulcers, or irritable bowel syndrome.
Causes of Gastroparesis
Gastroparesis can occur for various reasons, though some causes are better understood than others. Here are the most common:
Diabetes-Related Nerve Damage
Diabetes—especially when poorly controlled—is the leading cause of gastroparesis. High blood sugar levels damage nerves throughout the body, including the vagus nerve responsible for stomach motility. What is Diabetic Gastroparesis Symptoms, Causes and Treatment
Post-Surgical Nerve Injury
Surgeries involving the stomach, esophagus, or nearby organs may accidentally harm nerves, leading to delayed gastric emptying.
Viral or Bacterial Infections
Some people develop gastroparesis after a severe infection that disrupts the digestive system.
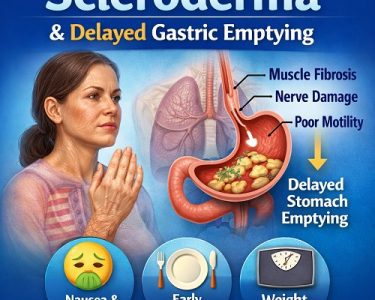
Autoimmune Conditions
Diseases like lupus, rheumatoid arthritis, and scleroderma can attack the nerves and muscles of the gastrointestinal tract.
Thyroid and Hormonal Disorders
Hypothyroidism, hormonal imbalances, and endocrine disorders may also influence digestive speed.
Medication-Induced Gastroparesis
Certain medications slow down digestion, including opioids, antidepressants, and some antihistamines. Recent research even highlights how weight loss pills may lead to stomach paralysis, finds new study, raising concerns about medication-related gastric slowdowns.
Idiopathic (Unknown Causes)
Up to 40% of cases have no clear reason, making diagnosis and treatment even more challenging.
Common Symptoms of Gastroparesis
Gastroparesis presents itself in various ways, and symptoms may come and go. The most frequent include:
- Persistent nausea
- Vomiting undigested food
- Early fullness during meals
- Upper abdominal bloating
- Heartburn or acid reflux
- Poor appetite
- Irregular blood sugar levels
- Stomach pain or cramping
- Difficulty digesting high-fiber or high-fat foods
While many people assume gastroparesis always leads to weight loss, this is not true for everyone. In fact, many patients experience weight gain gastroparesis symptoms due to hormonal shifts, altered eating habits, and slowed metabolism.
Why Weight Gain Happens With Gastroparesis
The connection between weight gain and gastroparesis is more common than most people think. Although the condition causes slow digestion, the body often reacts in ways that unintentionally promote weight gain.
Let’s break down why this happens.
Changes in Eating Patterns
People with gastroparesis often adapt their eating habits to avoid discomfort. They may:
- Eat smaller but more frequent meals
- Choose soft, processed, or liquid foods
- Avoid fibrous vegetables and lean proteins
- Rely on calorie-dense snacks to boost energy
These adjustments, especially frequent snacking, can lead to higher calorie intake despite reduced digestion efficiency.
Patients commonly ask, “can gastroparesis cause weight gain”, and the answer is yes—especially when the body compensates for slow digestion by craving easily digestible, high-calorie foods.
Reduced Physical Activity
Gastroparesis often causes fatigue, weakness, and abdominal discomfort. Many individuals become less active due to fear of worsening symptoms or because they simply feel unwell.
A reduction in activity slows metabolism, making it easier to gain weight even when eating less.
This leads many to wonder: does gastroparesis cause weight gain even when they are careful? Reduced movement, combined with slower digestion, absolutely contributes.
Hormonal and Metabolic Changes
The stomach plays a surprisingly large role in metabolic regulation. Delayed emptying changes how hormones like insulin, ghrelin, and leptin function.
- Ghrelin (the hunger hormone) becomes imbalanced
- Insulin resistance may increase
- Blood sugar fluctuations trigger cravings
These hormonal shifts explains why can gastroparesis cause you to gain weight is a question many patients ask their doctors.
High-Calorie Liquid Diets
When solid foods trigger symptoms, many people switch to smoothies, shakes, and liquid nutrition drinks. While easier to digest, liquid nutrition is often high in sugar and calories.
These calorie-dense liquids can cause significant weight gain over time.
Emotional Eating and Stress Response
Chronic conditions like gastroparesis increase stress, anxiety, and frustration. Emotional eating or comfort eating becomes a coping mechanism for some individuals.
This emotional response may answer the question: can gastroparesis symptoms cause weight gain? For many, the emotional toll contributes to weight fluctuations.
Gastroparesis Symptoms Often Misinterpreted as Weight Gain
Sometimes, what feels like weight gain is actually:
- Fluid retention
- Severe bloating
- Food lingering in the stomach
- Constipation
This can make patients feel heavier even without actual fat gain. The sensation is uncomfortable, but it is important to distinguish between true weight gain and digestive fullness caused by gastroparesis.
Who Is Most at Risk of Weight Gain With Gastroparesis?
While anyone with gastroparesis may experience weight gain, it is more common in:
People With Diabetes
Blood sugar swings increase hunger and energy crashes.
Individuals With Hormonal Imbalances
Conditions like hypothyroidism slow metabolic processes.
Patients on Certain Medications
Drugs that affect appetite, digestion, or fluid retention contribute significantly.
Those Following Liquid-Only Diets
High-calorie shakes are easier to digest but often nutritionally imbalanced.
Individuals With Anxiety or Emotional Eating Habits
Stress eating is a major factor.
Understanding the Emotional Side of Gastroparesis and Weight Gain
Weight gain can be mentally exhausting for patients who expect to lose weight because of chronic nausea and early satiety. They may feel confused or frustrated when the scale rises despite eating less.
Key emotional struggles include:
- Feeling misunderstood
- Fear that doctors may not take symptoms seriously
- Body image challenges
- Shame around eating habits
- Confusion about metabolic changes
Acknowledging these psychological aspects is crucial for healing and overall well-being.
How Doctors Diagnose Gastroparesis
Even though this guide focuses on the condition itself rather than management methods, it helps to understand the diagnostic tools used:
Gastric Emptying Study (GES)
This is the most common test. Patients eat a small meal with a safe radioactive marker, and the scan measures how long it takes to empty the stomach.
Upper Endoscopy
Used to rule out blockages or ulcers.
Smart Pill Test
A small electronic capsule tracks movement through the digestive tract.
Ultrasound or CT Scan
These rule out gallbladder disease and other digestive issues.
Blood Tests
These check thyroid levels, glucose control, and signs of infection.
Understanding the diagnostic process helps patients make sense of their symptoms and confirms whether weight gain and gastroparesis are linked in their case.
What Happens If Gastroparesis Is Not Managed?
Unmanaged gastroparesis may lead to:
- Severe dehydration
- Malnutrition
- Electrolyte imbalances
- Blood sugar instability
- Persistent nausea and vomiting
- Worsening weight gain or weight loss
- Increased risk of bezoars (undigested food masses)
Some patients explore options like natural remedies for gastroparesis or Natural supplements for gastroparesis as supportive measures, though lifestyle changes and medical care remain essential.
Important Note About Medications and Treatments
While this article is focused on describing the disease itself, some readers may be curious about treatment options. Medications such as prokinetics, anti-nausea drugs, and gastric therapies may be part of a doctor-recommended plan. This is where options like the best medications for gastroparesis treatment come into play for symptom relief.
These treatment options should always be discussed with a healthcare provider for personalized guidance.
Conclusion: Understanding the Link Between Weight Gain and Gastroparesis
Although many people assume gastroparesis always leads to weight loss, it can absolutely contribute to weight gain in various ways. Changes in metabolism, digestion, hormones, emotional state, and eating patterns all play a major role.
Recognizing the signs early helps patients understand what their body is going through. Whether the concern is nausea, fullness, bloating, or weight gain and gastroparesis, understanding the root of the problem is the first step toward long-term health transformation.
Gastroparesis is complex—but with the right knowledge, support, and medical care, it is absolutely manageable. Awareness is power, and understanding your symptoms is the key to taking control of your digestive health.