Gastroparesis is a chronic gastrointestinal condition that affects millions of people worldwide, yet it is still widely misunderstood. Before exploring is gastroparesis a disability, it is essential to understand the disease itself—what happens inside the digestive system, why it occurs, and how it impacts daily life. This foundational knowledge clarifies why many individuals with this condition struggle physically, emotionally, and socially.
Early in the journey of symptoms, many people wonder can stress cause gastroparesis? because the onset can feel sudden or unexplained. While stress alone is not typically the root cause, it can intensify symptoms and worsen the patient’s quality of life. To fully understand how debilitating this condition can be, we must begin by examining what gastroparesis actually is.
Understanding Gastroparesis: A Chronic Digestive Disorder
Gastroparesis is a medical condition where the stomach muscles weaken or become partially paralyzed, preventing the stomach from emptying food into the small intestine at the normal rate. This slowdown or stoppage of gastric motility is not caused by a physical blockage but rather a malfunction of the stomach muscles or the nerves responsible for regulating digestive movements.
The most commonly affected nerve is the vagus nerve, which controls contraction of the stomach muscles. When damaged or impaired, the stomach loses its ability to process and push food forward. This leads to delayed gastric emptying, a hallmark feature of gastroparesis.
People often first learn about this condition during major life events such as gastroparesis and pregnancy, where hormonal changes may influence gastrointestinal motility. Although pregnancy itself doesn’t cause gastroparesis, some individuals notice flare-ups or symptom intensification, prompting further medical evaluation.
How Gastroparesis Develops: The Biological Breakdown
To understand why gastroparesis happens, it helps to know how a healthy digestive system works. Normally, the stomach contracts rhythmically to grind and move food into the small intestine. These contractions depend on strong, coordinated muscle movements and healthy nerve signals. When any part of this process is disrupted, gastroparesis can develop.
The Role of the Vagus Nerve
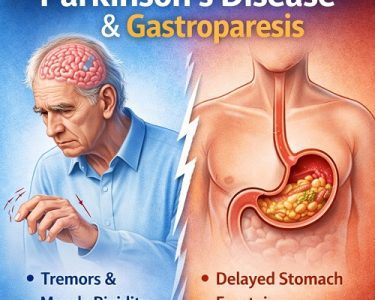
The vagus nerve serves as a communication highway between the brain and the digestive tract. It signals the stomach muscles to contract and move food along. When this nerve becomes damaged—due to diabetes, viral infections, surgery, or autoimmune activity—its ability to coordinate movement weakens.
Muscle Dysfunction in the Stomach
If the stomach muscles themselves are diseased or weakened, they cannot effectively grind or transfer food. This leads to stagnation, fermentation, bloating, and delayed emptying.
Electrical Rhythm Disturbances
The stomach relies on electrical signals, generated by specialized cells called ICCs (Interstitial Cells of Cajal), to regulate motility. A deficiency or malfunction in these cells can also result in gastroparesis.
What Causes Gastroparesis? Understanding the Underlying Factors
Researchers continue to uncover new causes of gastroparesis, but the following are the most recognized:
Diabetes
Diabetes is the leading cause of gastroparesis worldwide. Elevated blood sugar levels damage nerves over time—including the vagus nerve. People with long-standing or poorly controlled diabetes are especially at risk.
Post-Surgical Nerve Injury
Surgeries involving the stomach, esophagus, or intestines may inadvertently injure the vagus nerve, leading to motility issues later.
Viral Infections
Some individuals develop gastroparesis following viral illnesses. These infections can temporarily or permanently interfere with nerve signaling.
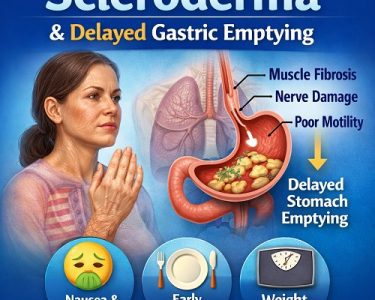
Autoimmune Disease
Conditions like scleroderma or lupus may attack the nerves or muscles responsible for stomach contractions.
Medications
Certain medications—such as opioids, antidepressants, and some blood pressure drugs—slow the digestive process and may trigger gastroparesis-like symptoms.
Idiopathic Causes
Many cases remain classified as idiopathic gastroparesis, meaning the cause is unknown. This often leads to frustration and delayed diagnosis.
Symptoms of Gastroparesis: How to Spot Them Before It’s Too Late
One of the biggest challenges in diagnosing gastroparesis is that its symptoms overlap with many other gastrointestinal conditions. Some people may wonder how to spot them before it’s too late, especially because early symptoms are often dismissed as common indigestion. Recognizing early warning signs can be life-changing.
Persistent Nausea
Nausea is one of the most common symptoms and may worsen after eating.
Vomiting Undigested Food
Since the stomach struggles to empty properly, food may remain for hours or even days, leading to vomiting of undigested material.
Early Satiety
Patients feel full after eating only a small amount of food, which often leads to inadequate calorie intake.
Bloating and Abdominal Pain
Trapped food and delayed digestion cause gas buildup and significant discomfort.
Unintended Weight Loss
Prolonged difficulty eating and absorbing nutrients may lead to malnutrition.
Fluctuating Blood Sugar Levels
In diabetic patients, delayed digestion can cause dangerous highs and lows in blood sugar.
Daily Challenges: The Real-Life Burden of Gastroparesis
Gastroparesis is more than a digestive issue—it affects every aspect of daily living. Eating becomes physically and emotionally stressful. The social aspect of food, celebrations, and family life is disrupted. Many patients struggle with fatigue, anxiety, and depression.
In severe cases, complications such as dehydration, electrolyte imbalance, and malnutrition can become life-threatening. Some people even question what is the average gastroparesis life expectancy? as they navigate the chronic and unpredictable nature of the disease. Although gastroparesis itself is not considered fatal, complications can affect long-term health.
Is Gastroparesis a Disability? Understanding the Legal and Medical Perspective
Now that we understand the severity of the condition, it becomes easier to explore the question: is gastroparesis a disability?
The answer is: It can be—depending on the severity and impact on daily functioning.
Gastroparesis affects each person differently. Some individuals manage symptoms well with dietary adjustments, while others may be unable to work, maintain normal daily activities, or meet nutritional needs without medical support. This leads many people to ask questions related to gastroparesis disability, including qualification rules, evidence requirements, and long-term support options.
When Does Gastroparesis Qualify as a Disability?
Gastroparesis may qualify as a disability when:
- The symptoms are severe and persistent
- The condition limits major life activities (eating, digesting, working, standing, or daily mobility)
- Treatments do not adequately control symptoms
- The individual experiences consistent complications, such as dehydration or malnutrition
- Feeding tubes, IV nutrition, or hospitalization becomes necessary
Social security systems in many countries require proof that the condition significantly limits functional ability. This is why people frequently ask whether is gastroparesis considered a disability under specific medical guidelines. Documentation from gastroenterologists, dietitians, and primary care physicians is crucial.
Is Gastroparesis a Disabling Disease? Exploring Severity
Another commonly searched phrase is is gastroparesis a disabling disease, and the answer depends on the individual case. Gastroparesis becomes disabling when:
- It prevents the person from maintaining employment
- It disrupts nutrient absorption
- Eating becomes painful or nearly impossible
- Symptoms require constant medical monitoring
- Complications become recurrent or severe
Some individuals require:
- Gastric pacemakers
- Feeding tubes (J-tube or G-J tube)
- Intravenous nutrition (TPN)
- Frequent emergency care
These situations clearly demonstrate the disabling nature of the disease.
Risk Factors: Who Is Most Likely to Develop Gastroparesis?
Understanding risk factors is a critical part of early detection.
Diabetic Patients
Especially those with uncontrolled blood sugar.
Post-Surgery Individuals
Abdominal or thoracic surgery increases risk.
Women
Research shows gastroparesis occurs more commonly in women than men.
Autoimmune Disorders
These may disrupt nerve or muscle function.
Medication Use
Long-term use of certain drugs slows stomach motility.
Early Detection: Why It Matters
Detecting gastroparesis early allows better symptom management, prevents malnutrition, and improves quality of life. Patients who learn about symptoms early often ask about lifestyle changes such as diet tips for gastroparesis, which can help reduce discomfort before the condition progresses. If symptoms intensify, supportive options like Natural supplements for gastroparesis may be discussed with healthcare providers.
Conclusion: The Truth About Gastroparesis and Disability
Gastroparesis is a complex, often debilitating condition that can severely disrupt daily life. Understanding the disease—its causes, symptoms, risk factors, and complications—helps clarify why many people ask is gastroparesis a disability and whether they qualify for medical or financial support.
While not every case qualifies as a disability, many individuals experience profound limitations that make working, eating, and functioning normally extremely challenging. With early detection, proper management, nutritional planning, and medical monitoring, patients can significantly improve their quality of life.
Gastroparesis is not simply a stomach condition—it is a chronic disorder that affects the entire body and mind. Recognizing its severity is essential for patients, caregivers, employers, and healthcare professionals. If you or someone you love is experiencing symptoms, early evaluation is the key to understanding the condition and protecting long-term health.