Gastroparesis is a chronic digestive condition that affects the normal movement of the stomach muscles. When the stomach cannot empty food properly or efficiently, a wide range of uncomfortable and sometimes debilitating symptoms can develop. Recognizing Gastroparesis Symptoms early is essential for timely diagnosis, proper management, and prevention of complications.
In this comprehensive guide, we will explore Gastroparesis Symptoms in detail — from early warning signs to advanced manifestations. We will also discuss causes, risk factors, complications, and when to seek medical attention.
What Is Gastroparesis?
Gastroparesis, often referred to as delayed gastric emptying, occurs when the stomach muscles do not function properly. Normally, strong muscular contractions move food from the stomach into the small intestine. In gastroparesis, these contractions slow down or stop entirely, even though there is no physical blockage.
Because digestion is delayed, food remains in the stomach longer than it should. This leads to a buildup of pressure, fermentation of food, and various digestive disturbances. Understanding the progression of Gastroparesis Symptoms can help patients recognize the condition early.
Why Recognizing Gastroparesis Symptoms Matters
Early identification of Gastroparesis Symptoms allows for:
- Faster medical evaluation
- Dietary and lifestyle adjustments
- Prevention of malnutrition
- Better blood sugar control (especially in diabetic patients)
- Reduced risk of severe complications
Unfortunately, early symptoms are often mild or mistaken for common digestive issues such as indigestion or acid reflux.
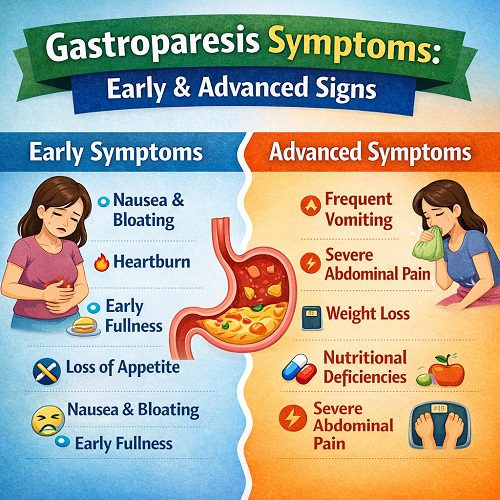
Early Gastroparesis Symptoms
Early Gastroparesis Symptoms can be subtle. They may appear intermittently and worsen gradually over time.
1. Mild Nausea
One of the first signs is occasional nausea, especially after meals. You may feel slightly queasy or uncomfortable shortly after eating. This happens because food is not moving efficiently through the stomach.
Unlike stomach flu or food poisoning, this nausea tends to recur frequently and is not accompanied by fever or acute illness.
2. Feeling Full Quickly (Early Satiety)
Early satiety is a hallmark of early Gastroparesis Symptoms. You may feel full after eating only a few bites of food.
This occurs because the stomach is not emptying properly. Even small amounts of food create pressure and fullness.
People often notice:
- Inability to finish regular meals
- Reduced appetite
- Gradual decrease in food intake
3. Bloating
Bloating is another common early symptom. Food sitting in the stomach ferments and produces gas, leading to abdominal distension.
You may experience:
- Tightness in the upper abdomen
- Visible swelling
- Discomfort after meals
This bloating may worsen throughout the day.
4. Mild Abdominal Discomfort
Early-stage gastroparesis can cause vague upper abdominal pain or discomfort. It may feel like:
- A dull ache
- Burning sensation
- Pressure in the stomach area
This discomfort is usually not severe initially but may increase as the condition progresses.
5. Heartburn or Acid Reflux
Delayed gastric emptying increases pressure inside the stomach. This can cause stomach acid to move upward into the esophagus, leading to:
- Heartburn
- Sour taste in the mouth
- Acid reflux symptoms
Many patients initially believe they have simple reflux disease rather than gastroparesis.
6. Occasional Vomiting
In early stages, vomiting may occur occasionally, particularly after large meals. Vomited material may contain undigested food consumed hours earlier.
This is an important clue that digestion is delayed.
Intermediate Gastroparesis Symptoms
As the condition progresses, Gastroparesis Symptoms become more frequent and more disruptive to daily life.
1. Frequent Nausea
Nausea becomes more persistent and may occur daily. It may worsen after eating solid foods, especially high-fat or high-fiber meals.
Chronic nausea can significantly affect quality of life and mental health.
2. Recurrent Vomiting
Vomiting becomes more frequent and may involve:
- Undigested food eaten several hours earlier
- Large volumes of stomach contents
- Relief of pressure after vomiting
Some patients vomit several times per week.
3. Significant Bloating
Bloating becomes more noticeable and uncomfortable. Clothes may feel tight, and the abdomen may appear distended.
Gas buildup and delayed emptying intensify this symptom.
4. Loss of Appetite
Due to persistent nausea and fullness, appetite declines significantly. Eating becomes unpleasant or associated with discomfort.
Patients may skip meals or avoid eating entirely.
5. Unintentional Weight Loss
As food intake decreases and vomiting increases, weight loss becomes evident. This is one of the more concerning Gastroparesis Symptoms because it can lead to nutritional deficiencies.
6. Blood Sugar Fluctuations (Especially in Diabetics)
For individuals with diabetes, gastroparesis can cause unpredictable blood sugar levels.
Because food remains in the stomach longer:
- Blood sugar may drop initially.
- It may spike later when delayed food suddenly empties.
This makes glucose management extremely challenging.
Advanced Gastroparesis Symptoms
Advanced Gastroparesis Symptoms can become severe and potentially life-threatening if left untreated.
1. Severe Vomiting
Vomiting may occur daily or multiple times per day. It can lead to:
- Dehydration
- Electrolyte imbalance
- Weakness
- Hospitalization
Vomiting may also contain bile or partially digested food from many hours prior.
2. Malnutrition
Chronic inability to eat or absorb nutrients properly leads to malnutrition. Signs include:
- Muscle weakness
- Fatigue
- Hair thinning
- Dry skin
- Vitamin deficiencies
Malnutrition significantly weakens the immune system.
3. Dehydration
Frequent vomiting and poor oral intake can result in dehydration, which may cause:
- Dizziness
- Dark urine
- Dry mouth
- Rapid heartbeat
- Low blood pressure
Severe dehydration requires urgent medical attention.
4. Formation of Bezoars
When food remains in the stomach for prolonged periods, it can harden into a mass called a bezoar.
Bezoars can:
- Cause stomach obstruction
- Increase nausea and vomiting
- Block food passage entirely
This is a serious complication of advanced gastroparesis.
5. Severe Abdominal Pain
Pain may intensify due to pressure, inflammation, or complications like bezoars. Persistent or worsening abdominal pain should not be ignored.
6. Depression and Anxiety
Chronic digestive discomfort, dietary restrictions, and fear of vomiting can severely affect mental health.
Advanced Gastroparesis Symptoms often lead to:
- Social withdrawal
- Anxiety around eating
- Emotional distress
- Depression
Mental health support is often an essential part of treatment.
Causes of Gastroparesis
Understanding causes helps explain why Gastroparesis Symptoms develop.
Common causes include:
1. Diabetes
High blood sugar can damage the vagus nerve, which controls stomach muscles.
2. Nerve Damage
Surgery or trauma affecting the stomach or vagus nerve can disrupt gastric movement.
3. Viral Infections
Certain viral illnesses may temporarily or permanently affect stomach nerves.
4. Medications
Some medications slow stomach emptying, including:
- Opioids
- Antidepressants
- Certain blood pressure drugs
5. Autoimmune Disorders
Autoimmune conditions may attack nerves involved in digestion.
6. Idiopathic Causes
In many cases, no clear cause is identified.
How Gastroparesis Symptoms Differ from Other Digestive Disorders
Gastroparesis is often confused with:
- Acid reflux
- Irritable bowel syndrome
- Peptic ulcers
- Functional dyspepsia
Key distinguishing features include:
- Vomiting undigested food hours after eating
- Early satiety
- Severe bloating after small meals
- Delayed gastric emptying confirmed by testing
When to See a Doctor
Seek medical attention if you experience:
- Persistent nausea and vomiting
- Vomiting undigested food
- Unexplained weight loss
- Signs of dehydration
- Severe abdominal pain
- Blood sugar instability (if diabetic)
Early intervention can prevent worsening Gastroparesis Symptoms.
Complications of Untreated Gastroparesis
Ignoring Gastroparesis Symptoms can lead to:
- Severe malnutrition
- Dangerous blood sugar swings
- Chronic dehydration
- Stomach obstruction
- Repeated hospitalizations
- Reduced quality of life
Managing Gastroparesis Symptoms
Although there is no complete cure, many treatments can significantly improve symptoms.
1. Dietary Changes
Patients are often advised to:
- Eat small, frequent meals
- Avoid high-fat foods
- Limit high-fiber foods
- Choose soft or liquid foods
- Chew thoroughly
Liquid nutrition is often better tolerated.
2. Blood Sugar Control
For diabetic patients, careful glucose management is crucial.
3. Medications
Doctors may prescribe medications to:
- Stimulate stomach muscle contractions
- Reduce nausea
- Improve gastric emptying
4. Feeding Tubes or Nutritional Support
In severe cases, temporary or permanent feeding support may be necessary.
5. Surgical Options
Advanced cases may require surgical interventions or gastric electrical stimulation.
Living with Gastroparesis
Living with chronic Gastroparesis Symptoms can be challenging. Practical strategies include:
- Keeping a food diary
- Planning small meals
- Staying hydrated
- Working with a dietitian
- Seeking mental health support
- Joining support groups
With proper management, many patients experience symptom improvement.
Frequently Asked Questions About Gastroparesis Symptoms
Can Gastroparesis Symptoms come and go?
Yes. Symptoms may fluctuate, especially in early stages. Stress, illness, or diet changes can trigger flare-ups.
Are Gastroparesis Symptoms permanent?
Some cases are temporary, especially those caused by infections. However, many cases are chronic and require long-term management.
Is gastroparesis life-threatening?
While not usually immediately life-threatening, complications such as malnutrition, dehydration, and uncontrolled diabetes can become serious.
Final Thoughts
Gastroparesis Symptoms range from mild nausea and early fullness to severe vomiting, malnutrition, and dehydration. Recognizing early signs is critical for preventing progression and avoiding complications.
If you experience ongoing digestive discomfort, frequent nausea, or vomiting undigested food hours after eating, it is important to seek medical evaluation. Early diagnosis allows for better symptom management and improved quality of life.
Understanding Gastroparesis Symptoms empowers patients to take control of their health, seek appropriate care, and adopt lifestyle changes that reduce discomfort and improve overall well-being.