Obesity and severe gastrointestinal motility disorders represent two of the most challenging conditions in modern medicine. When lifestyle changes, medications, and less invasive therapies fail, advanced interventions may be necessary. Among these options, Gastric Electrical Stimulation has emerged as a promising therapeutic approach for carefully selected patients. Combined with or compared to traditional bariatric and gastrointestinal surgeries, Gastric Electrical Stimulation offers a unique, technology-driven pathway to symptom relief and metabolic improvement.
This article explores the science, surgical techniques, benefits, risks, and future outlook of Gastric Electrical Stimulation, and how it fits into the broader field of gastric surgery.
What Is Gastric Electrical Stimulation?
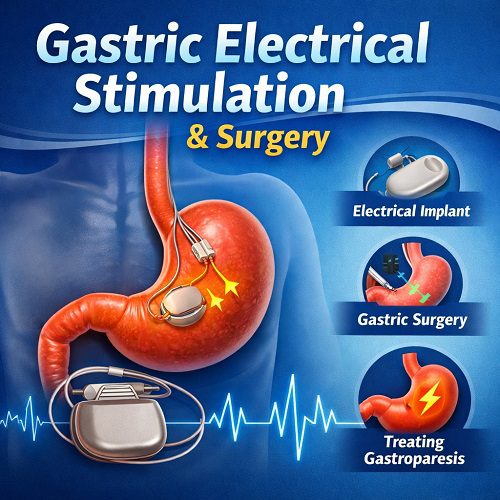
Gastric Electrical Stimulation (GES) is a medical therapy that uses mild electrical impulses delivered to the stomach muscles to improve gastric function. The therapy is performed by surgically implanting a small neurostimulator device—similar to a cardiac pacemaker—into the abdominal wall. Leads are attached to the muscular layer of the stomach, where they deliver controlled electrical pulses.
The primary goal of Gastric Electrical Stimulation is to:
- Improve gastric motility
- Reduce symptoms such as nausea and vomiting
- Enhance gastric emptying in selected cases
- Modulate appetite and satiety in obesity management
The device most commonly associated with this therapy is the Enterra Therapy System, which is FDA-approved under a Humanitarian Device Exemption for treatment of drug-refractory gastroparesis.
Medical Conditions Treated with Gastric Electrical Stimulation
1. Gastroparesis
Gastroparesis is a condition where the stomach empties food more slowly than normal without mechanical obstruction. It often occurs due to diabetes, post-surgical complications, or idiopathic causes.
Symptoms include:
- Chronic nausea
- Recurrent vomiting
- Bloating
- Early satiety
- Abdominal pain
- Malnutrition
Gastric Electrical Stimulation has shown significant symptom improvement in patients who do not respond to medications.
2. Obesity (Investigational and Adjunctive Use)
While bariatric surgery remains the gold standard for severe obesity, Gastric Electrical Stimulation has been investigated as a less invasive alternative or adjunct. By altering neural signaling in the stomach, it may:
- Promote early satiety
- Reduce caloric intake
- Influence hormonal pathways
Devices such as the Maestro Rechargeable System were developed to target vagal nerve pathways affecting appetite.
How Gastric Electrical Stimulation Works
The stomach’s normal function relies on coordinated electrical slow waves that regulate muscle contractions. In certain disorders, these rhythms become disrupted.
Gastric Electrical Stimulation works by:
- Delivering high-frequency, low-energy electrical pulses.
- Modulating gastric neural pathways.
- Reducing nausea signals transmitted to the brain.
- Potentially improving gastric accommodation.
Interestingly, the therapy does not always significantly accelerate gastric emptying. Instead, symptom relief appears to be mediated through neuromodulation mechanisms, influencing communication between the stomach and central nervous system.
The Surgical Procedure
Preoperative Evaluation
Before Gastric Electrical Stimulation surgery, patients typically undergo:
- Gastric emptying studies
- Endoscopy
- Nutritional assessment
- Psychological evaluation (especially in obesity cases)
- Medical therapy optimization
Only patients who have failed conservative management are considered candidates.
Implantation Procedure
The procedure is usually performed laparoscopically under general anesthesia.
Steps include:
- Small abdominal incisions are made.
- Two electrode leads are implanted into the muscular wall of the stomach.
- The stimulator device is placed in a subcutaneous pocket.
- The leads are connected to the device.
- The device is programmed externally.
Surgery typically lasts 1–2 hours, and most patients are discharged within 24–48 hours.
Gastric Electrical Stimulation vs. Traditional Gastric Surgery
To understand the role of Gastric Electrical Stimulation, it is helpful to compare it to conventional surgical procedures.
1. Gastric Bypass Surgery
The Roux-en-Y gastric bypass is one of the most common bariatric procedures. It reduces stomach size and reroutes the small intestine.
Key differences from Gastric Electrical Stimulation:
- Permanent anatomical alteration
- Significant weight loss outcomes
- Higher surgical risk
- Greater metabolic effects
2. Sleeve Gastrectomy
The Sleeve gastrectomy involves removing approximately 80% of the stomach.
Compared to Gastric Electrical Stimulation:
- Irreversible
- Highly effective for weight loss
- Alters hunger hormone ghrelin
- Greater long-term metabolic changes
3. Pyloroplasty
In gastroparesis cases, surgeons may perform Pyloroplasty to widen the pyloric channel and improve gastric emptying.
Unlike Gastric Electrical Stimulation, pyloroplasty directly modifies anatomy to facilitate food passage.
Advantages of Gastric Electrical Stimulation
1. Minimally Invasive
Because Gastric Electrical Stimulation does not require major anatomical alterations, it preserves normal gastric structure.
2. Reversible and Adjustable
The device can be:
- Reprogrammed externally
- Turned off
- Removed if necessary
This flexibility makes it appealing for patients hesitant about irreversible surgery.
3. Symptom Relief in Refractory Cases
Many patients with severe gastroparesis report substantial reductions in:
- Hospitalizations
- Vomiting episodes
- Need for parenteral nutrition
4. Lower Nutritional Deficiency Risk
Unlike bypass or sleeve procedures, Gastric Electrical Stimulation does not significantly impair nutrient absorption.
Risks and Complications
Although generally safe, Gastric Electrical Stimulation carries potential risks:
- Surgical site infection
- Lead displacement
- Device malfunction
- Abdominal pain
- Need for battery replacement
Battery life typically ranges from 5–10 years, after which replacement surgery is required.
Rare complications include bowel perforation or erosion of leads.
Effectiveness and Clinical Outcomes
For Gastroparesis
Studies show:
- Significant reduction in nausea and vomiting
- Improved quality of life
- Decreased hospitalization rates
However, improvement in gastric emptying time is inconsistent.
For Obesity
Weight loss results with Gastric Electrical Stimulation are generally modest compared to bariatric surgery. For this reason, it is not currently considered a first-line treatment for severe obesity.
Patient Selection Criteria
Ideal candidates for Gastric Electrical Stimulation typically:
- Have documented delayed gastric emptying
- Fail dietary and pharmacologic therapy
- Experience severe nausea and vomiting
- Are medically fit for surgery
For obesity treatment, candidates may:
- Have BMI 35–40 with comorbidities
- Prefer less invasive approaches
- Seek reversible interventions
Careful multidisciplinary evaluation is essential.
Recovery and Postoperative Care
Recovery after Gastric Electrical Stimulation surgery is generally smooth.
Postoperative considerations include:
- Device programming adjustments
- Gradual diet advancement
- Monitoring for infection
- Symptom tracking
Patients often require multiple follow-up visits to optimize stimulation settings.
Long-Term Management
Long-term success with Gastric Electrical Stimulation depends on:
- Ongoing device adjustments
- Management of underlying disease
- Nutritional support
- Monitoring psychological health
In diabetic gastroparesis, tight glycemic control is critical to maximize outcomes.
Future Directions in Gastric Electrical Stimulation
Research continues to refine Gastric Electrical Stimulation technology. Future innovations may include:
- Wireless devices
- Longer battery life
- Personalized stimulation algorithms
- Combined endoscopic implantation techniques
- Integration with digital health monitoring
Advancements in bioelectronic medicine may further expand the therapeutic applications of Gastric Electrical Stimulation beyond gastroparesis and obesity.
Ethical and Cost Considerations
The cost of Gastric Electrical Stimulation surgery can be substantial. Insurance coverage varies depending on indication and geographic location.
Because of its limited FDA approval under humanitarian exemption status, some patients may face barriers to access.
Healthcare providers must balance:
- Clinical benefit
- Economic cost
- Alternative treatment effectiveness
- Patient quality of life
Comparing Quality of Life Outcomes
Quality of life improvements are often more meaningful than objective gastric emptying metrics.
Patients frequently report:
- Reduced vomiting episodes
- Increased social functioning
- Improved nutritional status
- Less reliance on feeding tubes
When compared to major gastric surgeries, Gastric Electrical Stimulation offers symptom control without drastic anatomical changes.
Who Should Consider Gastric Electrical Stimulation?
Gastric Electrical Stimulation may be appropriate for:
- Patients with severe, medication-resistant gastroparesis
- Individuals experiencing repeated hospitalizations
- Patients unsuitable for major gastric resection
- Those seeking a reversible surgical option
It may not be ideal for:
- Mild gastroparesis
- Primary obesity without severe symptoms
- Patients unable to undergo anesthesia
The Role of Multidisciplinary Care
Successful Gastric Electrical Stimulation therapy requires collaboration among:
- Gastroenterologists
- Bariatric surgeons
- Endocrinologists
- Dietitians
- Psychologists
Integrated care ensures optimal patient selection and postoperative management.
Conclusion
Gastric Electrical Stimulation represents a sophisticated intersection of surgery and bioelectronic medicine. While not a replacement for traditional bariatric procedures like gastric bypass or sleeve gastrectomy, it plays a vital role in treating refractory gastroparesis and select metabolic conditions.
Its minimally invasive nature, reversibility, and neuromodulatory mechanism distinguish it from conventional gastric surgeries. However, patient selection, realistic expectations, and long-term follow-up are critical to success.
As technology evolves, Gastric Electrical Stimulation may become an increasingly refined and personalized therapeutic tool. For patients suffering from debilitating gastric disorders, it offers hope—bridging the gap between medical therapy and irreversible surgical intervention.