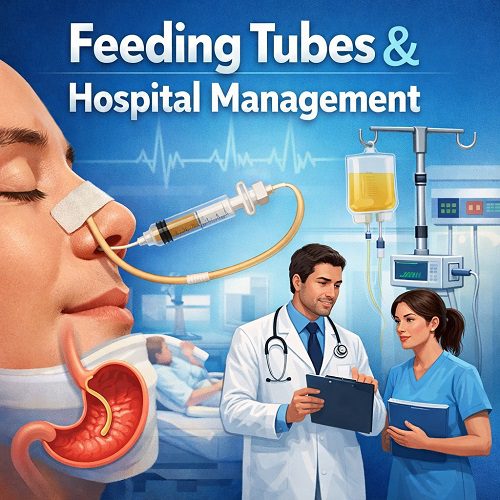
Feeding Tubes play a vital role in modern healthcare, particularly within hospital settings where patients may be unable to meet their nutritional needs independently. Proper nutrition is fundamental to healing, immune function, recovery time, and overall patient outcomes. When oral intake is insufficient or unsafe, Feeding Tubes become a life-sustaining intervention. However, their use extends beyond simple insertion and feeding. Effective hospital management of Feeding Tubes requires coordinated protocols, interdisciplinary collaboration, infection control measures, patient monitoring, and ethical considerations.
This article explores the clinical importance of Feeding Tubes, their types, indications, insertion procedures, complications, and the critical role hospital management plays in ensuring safe and effective nutritional support.
Understanding Feeding Tubes
Feeding Tubes are medical devices used to deliver nutrition directly into the gastrointestinal (GI) tract when a patient cannot eat or swallow safely. They are part of enteral nutrition therapy, which is preferred over parenteral (intravenous) nutrition when the digestive system is functional.
Why Feeding Tubes Are Necessary
Patients may require Feeding Tubes due to:
- Stroke or neurological disorders affecting swallowing (dysphagia)
- Head and neck cancers
- Severe trauma or burns
- Prolonged unconsciousness or coma
- Gastrointestinal obstruction
- Severe malnutrition
- Post-operative recovery in certain surgeries
In hospital environments, early nutritional intervention using Feeding Tubes has been associated with reduced infection rates, shorter hospital stays, and improved wound healing.
Types of Feeding Tubes
Hospital staff must understand the different types of Feeding Tubes to ensure appropriate selection and management.
1. Nasogastric (NG) Tubes
Inserted through the nose into the stomach, NG tubes are typically used for short-term feeding (less than 4–6 weeks). They are common in acute care settings and emergency situations.
Advantages:
- Easy bedside insertion
- Suitable for short-term use
- Cost-effective
Limitations:
- Risk of displacement
- Nasal irritation
- Increased aspiration risk if improperly positioned
2. Nasojejunal (NJ) Tubes
These Feeding Tubes pass through the nose into the jejunum (part of the small intestine). They are used when gastric feeding is not tolerated.
Advantages:
- Reduced aspiration risk
- Useful in cases of delayed gastric emptying
Limitations:
- More complex placement
- May require imaging confirmation
3. Gastrostomy Tubes (G-Tubes)
Placed directly into the stomach through the abdominal wall, gastrostomy Feeding Tubes are used for long-term nutritional support. They may be inserted surgically or endoscopically.
Advantages:
- Suitable for long-term feeding
- More comfortable than nasal tubes
Limitations:
- Risk of site infection
- Requires ongoing stoma care
4. Jejunostomy Tubes (J-Tubes)
Inserted directly into the jejunum, these Feeding Tubes are often used in patients with severe gastric dysfunction.
Hospital Protocols for Feeding Tubes
Hospital management plays a critical role in standardizing Feeding Tubes practices to minimize complications and improve patient outcomes.
Assessment Before Insertion
Before placing Feeding Tubes, healthcare providers assess:
- Nutritional status
- Swallowing function
- Gastrointestinal functionality
- Risk of aspiration
- Patient prognosis
Registered dietitians often collaborate with physicians to determine caloric and protein needs.
Insertion Guidelines
Hospitals typically maintain strict protocols for insertion, including:
- Verifying tube placement via X-ray (for NG/NJ tubes)
- Using sterile technique during surgical placements
- Monitoring vital signs during and after insertion
- Documenting procedure details in patient records
Misplacement of Feeding Tubes can lead to severe complications such as aspiration pneumonia or lung injury, making verification essential.
Nutritional Management and Monitoring
Once Feeding Tubes are placed, ongoing hospital management ensures appropriate nutritional delivery.
Developing a Feeding Plan
A multidisciplinary team—including physicians, nurses, and dietitians—creates individualized feeding regimens based on:
- Caloric needs
- Fluid requirements
- Medical condition
- Metabolic demands
- Lab values
Enteral formulas vary, including standard, high-protein, diabetic-specific, renal-specific, and immune-support formulas.
Monitoring Parameters
Hospitals monitor:
- Weight changes
- Electrolyte levels
- Blood glucose
- Hydration status
- Gastric residual volumes (in some cases)
- Signs of intolerance (vomiting, diarrhea, bloating)
Proper documentation and communication among staff prevent complications and ensure effective therapy.
Infection Control and Safety
Feeding Tubes introduce potential infection risks, particularly at insertion sites or through contamination of feeding systems.
Preventing Infections
Hospital infection control protocols include:
- Regular hand hygiene
- Sterile dressing changes
- Cleaning feeding ports before use
- Replacing feeding bags and tubing per guidelines
- Monitoring for redness, swelling, or discharge at stoma sites
Hospitals also train staff on proper flushing techniques to prevent tube blockages and bacterial growth.
Complications Associated with Feeding Tubes
Despite their benefits, Feeding Tubes may cause complications that require vigilant hospital oversight.
Mechanical Complications
- Tube dislodgement
- Blockage
- Kinking
- Leakage
Prompt detection and intervention prevent delays in nutrition.
Gastrointestinal Complications
- Nausea
- Diarrhea
- Constipation
- Abdominal distension
These issues often require formula adjustment or feeding rate modification.
Aspiration Pneumonia
One of the most serious risks of Feeding Tubes is aspiration. Hospitals implement measures such as:
- Elevating the head of the bed to 30–45 degrees
- Monitoring for coughing or respiratory distress
- Verifying tube placement regularly
Metabolic Complications
Electrolyte imbalances and refeeding syndrome can occur, particularly in severely malnourished patients. Hospital teams monitor laboratory values closely to adjust feeding rates gradually.
The Role of Nursing in Feeding Tubes Management
Nurses are central to daily Feeding Tubes care in hospital settings.
Their responsibilities include:
- Verifying tube placement before feeding
- Administering enteral nutrition and medications
- Flushing tubes appropriately
- Monitoring tolerance
- Educating patients and families
- Documenting intake and output
Nursing vigilance significantly reduces complications and ensures continuity of care.
Interdisciplinary Collaboration
Effective hospital management of Feeding Tubes depends on teamwork.
Key Team Members
- Physicians
- Registered dietitians
- Nurses
- Speech-language pathologists
- Pharmacists
- Infection control specialists
Speech-language pathologists assess swallowing ability to determine whether Feeding Tubes are necessary or if oral feeding can resume safely.
Pharmacists review medication formulations to ensure compatibility with enteral administration.
Ethical and Legal Considerations
Feeding Tubes sometimes raise ethical questions, particularly in end-of-life care.
Informed Consent
Hospitals must ensure:
- Clear explanation of benefits and risks
- Discussion of alternative options
- Respect for patient autonomy
Advance Directives
Some patients may have living wills addressing artificial nutrition. Hospital management teams must honor documented wishes and involve ethics committees when necessary.
Cultural Sensitivity
Cultural beliefs about artificial feeding may influence decision-making. Hospitals encourage culturally competent discussions with families.
Cost and Resource Management
Feeding Tubes also impact hospital resources and budgeting.
Cost Factors
- Tube placement procedures
- Enteral formulas
- Feeding equipment
- Staff time
- Complication management
Hospitals implement standardized feeding protocols to reduce unnecessary expenditures and improve efficiency.
Reducing Length of Stay
Proper nutritional support through Feeding Tubes can:
- Accelerate wound healing
- Improve immune response
- Decrease infection rates
- Shorten hospital stays
Efficient hospital management therefore supports both patient outcomes and financial sustainability.
Transitioning from Hospital to Home
Discharge planning is crucial when patients require long-term Feeding Tubes.
Education and Training
Before discharge, hospitals provide:
- Tube care instructions
- Feeding schedule guidance
- Emergency troubleshooting advice
- Infection warning signs
- Supply management training
Home health services may be arranged to support patients and caregivers.
Follow-Up Care
Regular outpatient follow-up ensures:
- Nutritional adequacy
- Tube integrity
- Weight monitoring
- Lab assessment
Hospitals coordinate with community healthcare providers to maintain continuity.
Quality Improvement in Hospital Management
Hospitals continually evaluate Feeding Tubes practices through:
- Audits
- Infection tracking
- Complication reporting
- Staff training programs
- Patient satisfaction surveys
Quality improvement initiatives often focus on reducing aspiration rates, minimizing tube dislodgement, and enhancing documentation accuracy.
Electronic medical records also support standardized Feeding Tubes protocols and automated reminders for monitoring.
Technological Advances in Feeding Tubes
Advancements are improving safety and efficiency.
Innovations Include:
- Radiopaque tubes for easier imaging confirmation
- Anti-clogging designs
- Closed feeding systems to reduce contamination
- Smart pumps with rate control and alarm systems
Hospitals adopting advanced technologies often see reductions in error rates and improved patient safety.
Risk Management and Legal Protection
Hospitals must document all Feeding Tubes procedures thoroughly to reduce legal risk.
Key documentation elements include:
- Informed consent
- Placement verification
- Feeding tolerance
- Complication management
- Patient education
Failure to adhere to protocol can lead to malpractice claims, particularly in cases of aspiration or improper tube placement.
Special Populations
Pediatric Patients
In pediatric hospitals, Feeding Tubes are commonly used for congenital disorders, prematurity, or neurological impairments. Management requires growth tracking and family-centered education.
Geriatric Patients
Older adults frequently require Feeding Tubes due to stroke or dementia. Hospital management must weigh nutritional benefits against quality-of-life considerations.
Critically Ill Patients
In intensive care units (ICUs), early enteral nutrition through Feeding Tubes is standard practice. Continuous monitoring is essential to prevent complications in hemodynamically unstable patients.
Conclusion
Feeding Tubes are indispensable tools in modern hospital care, providing essential nutritional support for patients unable to eat independently. However, their success depends not only on proper placement but also on comprehensive hospital management strategies.
From insertion protocols and infection prevention to interdisciplinary collaboration and ethical oversight, hospitals must maintain rigorous standards to ensure safe and effective enteral nutrition. With structured policies, ongoing staff training, and quality improvement initiatives, Feeding Tubes can significantly enhance patient recovery, reduce complications, and improve overall healthcare outcomes.
As healthcare continues to evolve, advances in technology, education, and protocol development will further refine Feeding Tubes management, ensuring that patients receive the nutritional care necessary for healing and improved quality of life.