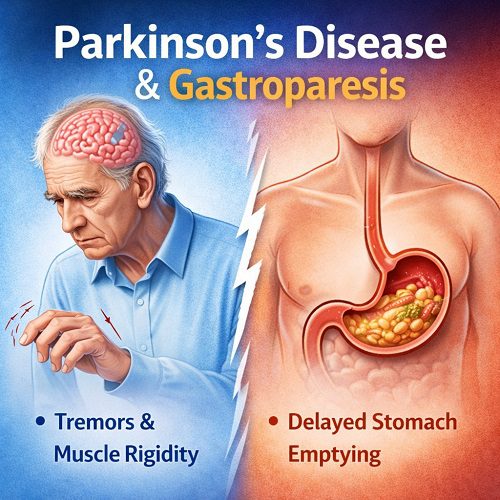
Parkinson’s Disease (PD) is a progressive neurodegenerative disorder primarily recognized for its motor symptoms, including tremors, rigidity, and bradykinesia. However, non-motor symptoms, particularly gastrointestinal issues, are increasingly acknowledged as significant contributors to reduced quality of life. Among these, Gastroparesis—a condition characterized by delayed gastric emptying—plays a critical role. Understanding the interplay between Parkinson’s Disease and gastroparesis is essential for early recognition, effective management, and improving patient outcomes.
What is Parkinson’s Disease?
Parkinson’s Disease is caused by the degeneration of dopamine-producing neurons in the substantia nigra region of the brain. Dopamine is a neurotransmitter essential for smooth, coordinated muscle movement. As these neurons deteriorate, motor and non-motor symptoms emerge.
Motor Symptoms of Parkinson’s Disease
The hallmark motor symptoms include:
- Tremor at rest: Often starting in one hand or limb.
- Bradykinesia: Slowness of movement affecting daily tasks.
- Rigidity: Muscle stiffness and reduced range of motion.
- Postural instability: Impaired balance and increased risk of falls.
- Masked face: Reduced facial expression.
Non-Motor Symptoms of Parkinson’s Disease
Non-motor symptoms can appear years before motor symptoms and significantly impact quality of life:
- Sleep disturbances (REM sleep behavior disorder)
- Cognitive impairment and dementia
- Mood disorders (depression and anxiety)
- Autonomic dysfunction (blood pressure fluctuations, sweating, constipation)
- Gastrointestinal issues, including gastroparesis
What is Gastroparesis?
Gastroparesis is a disorder in which the stomach empties food into the small intestine more slowly than normal without any mechanical obstruction. Symptoms may overlap with general digestive complaints but often include:
- Persistent nausea and vomiting
- Early satiety (feeling full quickly)
- Bloating and abdominal discomfort
- Weight loss in severe cases
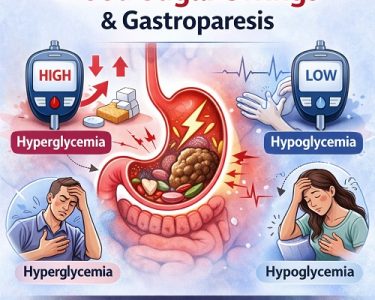
- Erratic blood sugar levels, especially in diabetic patients
In the context of Parkinson’s Disease, gastroparesis is primarily linked to autonomic nervous system dysfunction and impaired gastric motility.
The Link Between Parkinson’s Disease and Gastroparesis
Research indicates that gastrointestinal dysfunction is common in Parkinson’s Disease, affecting up to 80% of patients. The link is primarily attributed to:
- Autonomic Nervous System Dysfunction: PD affects the vagus nerve, which regulates stomach motility, leading to delayed gastric emptying.
- Alpha-Synuclein Aggregation: Misfolded alpha-synuclein proteins, a hallmark of PD, have been found in the enteric nervous system, suggesting that PD pathology extends to the gut.
- Medication Effects: Dopaminergic medications used to manage PD motor symptoms can exacerbate nausea and slow gastric emptying.
- Reduced Physical Activity: Motor limitations and bradykinesia may contribute indirectly to slower gastrointestinal motility.
This connection is significant because gastroparesis can affect the absorption of medications, including levodopa, reducing their effectiveness and worsening motor control.
Symptoms of Gastroparesis in Parkinson’s Disease
Gastrointestinal symptoms in PD are often subtle initially but may progress over time. Common signs of gastroparesis in PD patients include:
- Nausea and frequent vomiting
- Early fullness and bloating
- Abdominal discomfort or pain
- Weight loss and malnutrition
- Fluctuating responses to PD medications
- Constipation, which may coexist with delayed gastric emptying
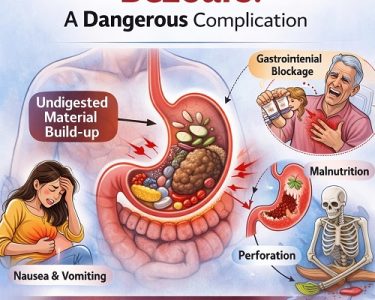
It’s important to recognize these symptoms early because untreated gastroparesis can lead to nutritional deficiencies and increased hospitalization risk.
Diagnosis of Gastroparesis in Parkinson’s Disease Patients
Diagnosing gastroparesis in Parkinson’s Disease requires careful evaluation to differentiate it from other gastrointestinal disorders. Common diagnostic approaches include:
- Medical History and Symptom Review: Understanding the pattern, timing, and triggers of digestive symptoms.
- Gastric Emptying Studies:
- Scintigraphy: The gold standard test for measuring the rate of stomach emptying.
- Breath Tests: Non-invasive method using labeled meals to assess gastric emptying.
- Endoscopy: Used to rule out mechanical obstruction or structural abnormalities.
- Imaging and Laboratory Tests: Assess nutritional status, electrolyte balance, and complications.
Early diagnosis is crucial because delayed gastric emptying can affect drug absorption, leading to fluctuations in PD symptom control.
Impact of Gastroparesis on Parkinson’s Disease Management
Gastroparesis can complicate PD management in several ways:
- Erratic Medication Absorption: Levodopa and other oral medications may have delayed or unpredictable absorption, resulting in “off” periods and worsening motor symptoms.
- Nutritional Deficiencies: Inadequate food intake can exacerbate fatigue, muscle weakness, and overall health.
- Increased Gastrointestinal Discomfort: Nausea and bloating can discourage eating, further affecting energy levels and medication efficacy.
Effective management of gastroparesis is therefore essential for optimizing both gastrointestinal and neurological outcomes in Parkinson’s Disease patients.
Treatment Approaches
Dietary and Lifestyle Modifications
- Eat smaller, more frequent meals to reduce gastric load.
- Favor low-fat and low-fiber foods that are easier to digest.
- Incorporate soft or liquid-based meals when symptoms are severe.
- Avoid lying down immediately after eating.
- Maintain adequate hydration.
Medications
- Prokinetic Agents: Medications like metoclopramide may improve gastric motility but should be used cautiously due to potential worsening of Parkinsonian symptoms.
- Anti-Nausea Medications: Ondansetron or domperidone can reduce nausea, but interactions with PD medications must be monitored.
- Adjustments in PD Medications: Timing and formulation changes, such as using liquid levodopa, can help compensate for delayed absorption.
Advanced Interventions
- Gastric Electrical Stimulation: Used in severe gastroparesis to enhance gastric contractions.
- Enteral Feeding: In extreme cases, feeding tubes may be necessary to maintain nutrition.
- Botulinum Toxin Injections: Occasionally used in specialized centers for pyloric relaxation.
The Role of Exercise and Physical Therapy
Physical activity can positively influence gastrointestinal motility. Recommendations include:
- Light to moderate aerobic exercise, such as walking or cycling.
- Stretching and flexibility exercises to reduce rigidity.
- Core strengthening to support digestive function.
Exercise also improves overall mobility, mood, and quality of life in Parkinson’s Disease patients.
Monitoring and Long-Term Management
Long-term management of Parkinson’s Disease with gastroparesis involves:
- Regular follow-ups with a neurologist and gastroenterologist.
- Monitoring nutritional status, weight, and hydration.
- Adjusting medications based on symptom fluctuations and gastric emptying rates.
- Tracking gastrointestinal symptoms and food intake through diaries or apps.
Patient education is critical: recognizing early signs of gastroparesis and understanding the impact on PD management can improve outcomes significantly.
Emerging Research and Future Directions
Recent studies suggest several promising areas of research:
- Gut-Brain Axis: Understanding how PD pathology affects the enteric nervous system may lead to novel treatments.
- Probiotic and Dietary Interventions: Modulating gut microbiota may help improve gastric motility and reduce inflammation.
- Advanced Drug Formulations: Research into alternative PD medication delivery methods (e.g., intestinal gels, subcutaneous pumps) aims to bypass delayed gastric emptying.
- Neuroprotective Therapies: Targeting alpha-synuclein aggregation may slow both neurological and gastrointestinal progression.
Complications if Left Untreated
Unmanaged gastroparesis in Parkinson’s Disease can lead to:
- Malnutrition and vitamin deficiencies (B12, iron)
- Dehydration and electrolyte imbalance
- Worsened motor symptoms due to inconsistent medication absorption
- Hospitalization due to severe nausea or weight loss
- Psychological stress, anxiety, and depression
Early intervention and comprehensive care can significantly reduce these risks.
Quality of Life Considerations
Gastroparesis significantly impacts daily living for PD patients:
- Difficulty maintaining a balanced diet
- Social limitations due to meal-related discomfort
- Increased fatigue and reduced physical activity
- Emotional distress related to chronic symptoms
Addressing gastroparesis proactively helps improve both the physical and psychological well-being of Parkinson’s Disease patients.
Patient Education and Support
Education is a cornerstone of managing Parkinson’s Disease and gastroparesis:
- Encourage patients to maintain food and symptom diaries.
- Provide guidance on meal planning and timing of medications.
- Support groups can offer practical advice and emotional support.
- Coordination between neurologists, gastroenterologists, dietitians, and primary care providers ensures holistic care.
Conclusion
The intersection of Parkinson’s Disease and Gastroparesis represents a complex clinical challenge. While Parkinson’s Disease is primarily a neurodegenerative disorder affecting motor function, its impact on the autonomic nervous system can lead to delayed gastric emptying, significantly influencing nutrition, medication efficacy, and overall quality of life.
Early recognition, comprehensive management, and patient education are essential for mitigating the impact of gastroparesis in Parkinson’s Disease. By combining dietary strategies, medication adjustments, exercise, and advanced interventions when necessary, patients can achieve improved symptom control and enhanced daily functioning. Ongoing research into the gut-brain connection holds promise for future therapies that may simultaneously target neurological and gastrointestinal aspects of Parkinson’s Disease.
Understanding and addressing the dual challenges of Parkinson’s Disease and Gastroparesis is not just about managing symptoms—it’s about empowering patients to maintain independence, dignity, and a better quality of life.