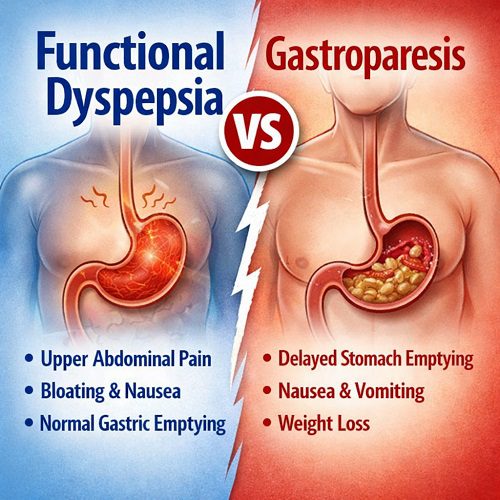
Functional dyspepsia and gastroparesis are two distinct gastrointestinal disorders that often confuse both patients and healthcare providers due to overlapping symptoms. While they affect digestion, the underlying causes, diagnostic criteria, and treatment approaches differ significantly. This article explores Functional Dyspepsia, compares it to Gastroparesis, and provides guidance on recognition, management, and improving quality of life for affected individuals.
What is Functional Dyspepsia?
Functional Dyspepsia (FD) is a chronic disorder characterized by upper abdominal discomfort or pain without an identifiable structural or biochemical cause. Unlike peptic ulcers or gastroesophageal reflux disease (GERD), functional dyspepsia occurs in the absence of visible damage to the stomach lining. The condition affects approximately 10–20% of the global population, making it one of the most common functional gastrointestinal disorders.
FD is often classified into two subtypes:
- Postprandial Distress Syndrome (PDS) – Marked by early satiety and post-meal fullness.
- Epigastric Pain Syndrome (EPS) – Characterized by pain or burning localized in the upper abdomen.
Symptoms may include:
- Upper abdominal discomfort or pain
- Bloating and fullness after meals
- Nausea and occasional vomiting
- Burping and belching
- Loss of appetite
These symptoms often fluctuate and can significantly impair daily activities, work productivity, and emotional well-being.
What is Gastroparesis?
Gastroparesis is a chronic disorder in which the stomach empties slowly due to impaired gastric motility, without any mechanical obstruction. The condition affects the stomach’s ability to move food into the small intestine, leading to a range of digestive issues. Gastroparesis is less common than functional dyspepsia but often causes more severe symptoms and complications.
Common causes of gastroparesis include:
- Diabetes mellitus – Particularly long-standing type 1 or type 2 diabetes
- Post-surgical complications – Especially after surgeries involving the stomach or vagus nerve
- Medications – Such as opioids or certain anticholinergics
- Idiopathic – In many cases, the cause is unknown
Symptoms overlap with FD but can be more severe:
- Persistent nausea and vomiting
- Early satiety and bloating
- Abdominal pain or discomfort
- Unintentional weight loss
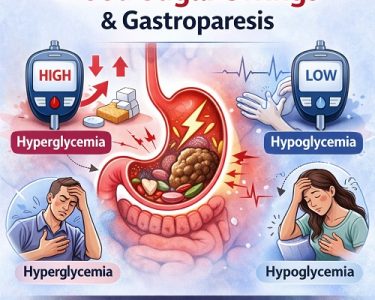
- Blood sugar fluctuations in diabetic patients
Unlike functional dyspepsia, gastroparesis can lead to malnutrition and electrolyte imbalances if left untreated.
Key Differences Between Functional Dyspepsia and Gastroparesis
Although both disorders involve upper gastrointestinal discomfort, their differences lie in pathology, diagnostic methods, and management. Here’s a detailed comparison:
Feature | Functional Dyspepsia | Gastroparesis |
| Definition | Chronic upper abdominal discomfort without structural abnormalities | Delayed gastric emptying due to impaired stomach motility |
| Cause | Multifactorial: visceral hypersensitivity, psychological factors, Helicobacter pylori infection, diet | Diabetes, post-surgical nerve damage, medications, idiopathic |
| Primary Symptoms | Early satiety, bloating, upper abdominal pain, nausea | Nausea, vomiting, early satiety, bloating, weight loss, fluctuating blood sugar |
| Gastric Emptying | Normal or minimally delayed | Significantly delayed |
| Diagnostic Tests | Clinical evaluation, endoscopy, H. pylori testing, gastric emptying studies (sometimes) | Gastric emptying scintigraphy, breath tests, electrogastrography |
| Treatment | Diet modification, acid suppression, prokinetics, psychological therapy | Prokinetics, dietary changes, glycemic control, gastric electrical stimulation in severe cases |
| Prognosis | Generally benign, though chronic | Can lead to complications if untreated, including malnutrition and hospitalization |
Causes and Risk Factors of Functional Dyspepsia
The exact cause of Functional Dyspepsia remains unclear, but research suggests a combination of factors:
- Visceral Hypersensitivity – Heightened sensitivity of the stomach lining to stretching and acid exposure.
- Delayed Gastric Emptying – Mild delays in gastric emptying may contribute to early fullness.
- Helicobacter pylori Infection – Some cases are linked to H. pylori, which can cause chronic inflammation.
- Stress and Psychological Factors – Anxiety, depression, and chronic stress often exacerbate symptoms.
- Lifestyle and Diet – High-fat meals, alcohol, caffeine, and irregular eating habits can worsen symptoms.
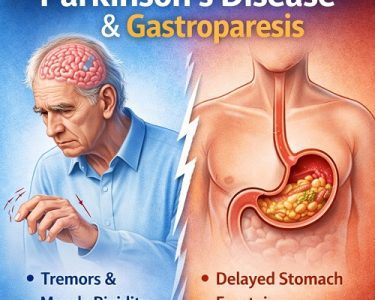
Causes and Risk Factors of Gastroparesis
Gastroparesis primarily results from impaired stomach motility caused by nerve or muscle dysfunction. Key risk factors include:
- Diabetes Mellitus – High blood glucose can damage the vagus nerve controlling stomach muscles.
- Surgery – Operations affecting the stomach or esophagus may damage nerves.
- Medications – Opioids, anticholinergics, and certain antidepressants can slow gastric emptying.
- Autoimmune Disorders – Conditions like scleroderma may affect stomach motility.
- Idiopathic Causes – In some cases, the exact reason remains unknown.
Symptoms Overlap: Why Confusion Occurs
Functional dyspepsia and gastroparesis share several symptoms, making diagnosis challenging:
- Early Satiety: Feeling full after eating small amounts.
- Bloating and Distension: Abdominal fullness and swelling.
- Nausea: Mild to severe, often triggered by meals.
- Abdominal Pain: Especially in the upper abdomen.
However, vomiting, significant weight loss, and blood sugar fluctuations are more indicative of gastroparesis.
Diagnostic Approaches
Functional Dyspepsia
Diagnosis of FD is primarily clinical, based on symptom patterns and exclusion of other conditions. Common diagnostic steps include:
- Medical History and Symptom Assessment: Frequency, timing, and triggers of symptoms.
- Endoscopy: To rule out ulcers, cancers, or structural abnormalities.
- H. pylori Testing: Breath, stool, or blood tests to detect infection.
- Gastric Emptying Studies: Occasionally used if delayed emptying is suspected.
Gastroparesis
Gastroparesis requires objective measurement of gastric emptying. Common tests include:
- Gastric Emptying Scintigraphy: Measures how long it takes for food to leave the stomach.
- Breath Tests: Non-invasive method using labeled meals.
- Electrogastrography: Monitors electrical activity of the stomach muscles.
- Imaging: To rule out obstructions.
Accurate diagnosis is crucial because management strategies differ significantly between FD and gastroparesis.
Treatment Strategies
Functional Dyspepsia Management
The primary goal is symptom relief and improving quality of life. Treatment may include:
- Dietary Modifications
- Eating smaller, frequent meals
- Avoiding high-fat, spicy, or acidic foods
- Reducing caffeine and alcohol intake
- Medications
- Proton Pump Inhibitors (PPIs): Reduce stomach acid
- H. pylori Eradication Therapy: If infection is present
- Prokinetics: Improve gastric motility in some patients
- Antidepressants: Low-dose tricyclic antidepressants or SSRIs to manage pain perception
- Psychological Therapies
- Cognitive-behavioral therapy (CBT)
- Stress management techniques
- Mindfulness and relaxation exercises
Gastroparesis Management
Gastroparesis treatment focuses on improving gastric emptying, controlling symptoms, and managing underlying causes:
- Dietary Adjustments
- Eating small, frequent meals
- Focusing on low-fat and low-fiber foods
- Pureed or liquid meals if severe
- Medications
- Prokinetic Drugs: Metoclopramide, domperidone to stimulate stomach contractions
- Antiemetics: Ondansetron or promethazine for nausea
- Glycemic Control
- Essential in diabetic gastroparesis
- Prevents further nerve damage
- Advanced Interventions
- Gastric Electrical Stimulation: For refractory cases
- Feeding Tubes or Parenteral Nutrition: In severe malnutrition
- Surgical Options: Rare, only if other interventions fail
Lifestyle Tips for Managing Symptoms
Both functional dyspepsia and gastroparesis can benefit from lifestyle adjustments:
- Maintain a food diary to identify triggers.
- Avoid lying down immediately after meals.
- Engage in regular mild exercise to improve digestion.
- Manage stress through meditation, yoga, or counseling.
- Avoid smoking, alcohol, and high-fat diets.
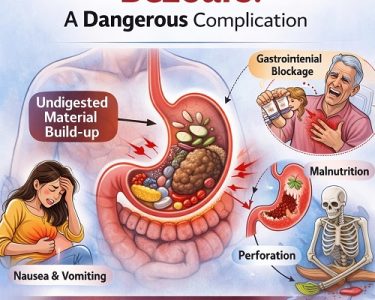
Complications
Functional Dyspepsia: Rarely leads to serious complications but can significantly affect quality of life, causing chronic discomfort, anxiety, and social limitations.
Gastroparesis: Can lead to more severe complications, such as:
- Malnutrition and weight loss
- Dehydration and electrolyte imbalance
- Poor glycemic control in diabetics
- Increased risk of hospitalization
Prognosis
Functional Dyspepsia generally has a favorable prognosis. Symptoms can fluctuate over time, and many patients find relief through lifestyle and dietary adjustments combined with medical therapy.
Gastroparesis tends to be chronic and may progressively worsen, especially in patients with diabetes. Early diagnosis and proactive management are crucial to prevent complications and maintain quality of life.
When to Seek Medical Attention
Seek professional evaluation if you experience:
- Persistent vomiting or unintentional weight loss
- Severe abdominal pain or bloating
- Difficulty swallowing
- Signs of dehydration
- Blood in vomit or stool
Early detection ensures appropriate differentiation between Functional Dyspepsia and Gastroparesis, guiding effective treatment.
Conclusion
Understanding the difference between Functional Dyspepsia and Gastroparesis is essential for accurate diagnosis and effective management. While both disorders involve upper gastrointestinal discomfort, functional dyspepsia is primarily a disorder of sensation and mild motility changes, whereas gastroparesis is defined by significant delayed gastric emptying and potential complications.
Proper evaluation, including symptom assessment and diagnostic testing, allows healthcare providers to tailor treatment strategies—from dietary modifications and medications to advanced interventions when necessary. Patients can significantly improve their quality of life by combining medical care with lifestyle adjustments, stress management, and careful monitoring of symptoms.
Ultimately, recognizing the unique features of each condition empowers patients and clinicians to manage these challenging gastrointestinal disorders more effectively, reducing discomfort, preventing complications, and enhancing overall well-being.