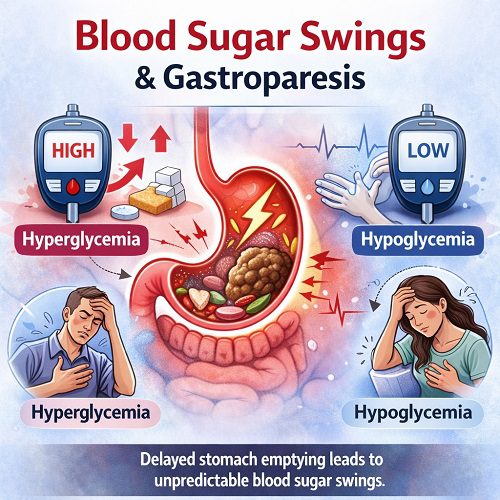
Managing digestive health can be challenging on its own—but when it intersects with blood glucose control, the complexity increases significantly. One of the most frustrating and potentially dangerous combinations is gastroparesis and Blood Sugar Swings. For individuals living with diabetes or other metabolic disorders, unpredictable digestion can lead to erratic glucose levels that are difficult to control.
In this comprehensive guide, we will explore the relationship between gastroparesis and Blood Sugar Swings, including causes, symptoms, complications, management strategies, and long-term outlook.
Understanding Gastroparesis
Gastroparesis is a digestive disorder in which the stomach empties food into the small intestine more slowly than normal. Unlike a blockage, there is no physical obstruction—rather, the stomach muscles fail to function properly.
The condition often develops when the vagus nerve, which controls stomach muscles, becomes damaged. This nerve damage is most commonly linked to long-standing diabetes, but gastroparesis can also occur after surgery, viral infections, or due to certain medications.
What Are Blood Sugar Swings?
Blood Sugar Swings refer to rapid or unpredictable fluctuations in blood glucose levels. Instead of remaining within a stable range, glucose levels may spike (hyperglycemia) or drop (hypoglycemia), sometimes within short periods.
Common signs of high blood sugar include:
- Excessive thirst
- Frequent urination
- Blurred vision
- Fatigue
Signs of low blood sugar may include:
- Shakiness
- Sweating
- Dizziness
- Confusion
- Rapid heartbeat
In individuals with gastroparesis, these fluctuations become even more difficult to predict and manage.
The Connection Between Gastroparesis and Blood Sugar Swings
The stomach plays a vital role in regulating glucose levels. Normally, food moves from the stomach into the small intestine at a steady rate, allowing glucose to enter the bloodstream gradually. Insulin or other medications are timed based on this predictable digestion process.
However, in gastroparesis:
- Food may remain in the stomach for hours.
- Glucose absorption becomes delayed.
- Insulin may act before glucose enters the bloodstream.
- Sudden emptying can cause rapid glucose spikes.
This disruption leads to severe Blood Sugar Swings, making diabetes management far more complicated.
Why Blood Sugar Swings Become Unpredictable
1. Delayed Gastric Emptying
When food lingers in the stomach, insulin taken before meals may lower blood sugar too early. This can result in hypoglycemia shortly after eating.
2. Sudden Gastric Emptying
At times, the stomach may suddenly release partially digested food into the small intestine. This can cause a rapid rise in blood glucose levels, leading to hyperglycemia.
3. Impaired Insulin Timing
Insulin dosing is typically calculated based on expected carbohydrate absorption. Gastroparesis disrupts this timing, making standard insulin regimens less effective.
4. Inconsistent Appetite
Nausea and early satiety can reduce food intake, making glucose control even less predictable.
Together, these factors create a cycle where gastroparesis worsens Blood Sugar Swings, and unstable blood sugar further damages stomach nerves.
The Vicious Cycle: High Blood Sugar Worsens Gastroparesis
The relationship between gastroparesis and Blood Sugar Swings is bidirectional.
- Chronic high blood sugar damages nerves, including the vagus nerve.
- Vagus nerve damage slows stomach emptying.
- Slowed stomach emptying causes erratic glucose absorption.
- Erratic glucose absorption causes more blood sugar instability.
Breaking this cycle is essential to preventing long-term complications.
Symptoms of Blood Sugar Swings in Gastroparesis
When gastroparesis and unstable glucose levels occur together, symptoms may overlap or intensify.
Digestive symptoms may include:
- Nausea
- Vomiting
- Bloating
- Abdominal pain
- Early fullness
Symptoms related to Blood Sugar Swings may include:
- Sudden fatigue
- Headaches
- Mood changes
- Sweating or chills
- Confusion
- Blurred vision
Patients often report feeling “out of control” regarding their diabetes management.
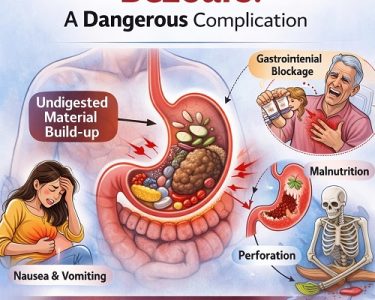
Complications of Uncontrolled Blood Sugar Swings
If not managed properly, repeated Blood Sugar Swings can lead to serious complications:
1. Severe Hypoglycemia
Dangerously low blood sugar can cause seizures, unconsciousness, or even death if untreated.
2. Chronic Hyperglycemia
Persistent high blood sugar increases the risk of:
- Kidney damage
- Nerve damage
- Eye disease
- Cardiovascular disease
3. Diabetic Ketoacidosis (DKA)
Extremely high blood sugar can lead to life-threatening metabolic imbalance.
4. Malnutrition
Gastroparesis may reduce nutrient absorption, compounding metabolic instability.
Diagnosing Gastroparesis in Patients with Blood Sugar Swings
Doctors may suspect gastroparesis when a patient with diabetes experiences unexplained Blood Sugar Swings despite consistent medication use.
Diagnostic tools include:
- Gastric emptying study
- Upper endoscopy
- Ultrasound or CT scan
- Blood glucose monitoring logs
Continuous glucose monitoring (CGM) devices are particularly helpful in identifying patterns.
Managing Blood Sugar Swings with Gastroparesis
Effective management requires a comprehensive approach.
1. Dietary Adjustments
Smaller, more frequent meals are recommended. Patients should:
- Avoid high-fat foods
- Limit high-fiber foods
- Choose soft or liquid meals
- Chew thoroughly
Liquid nutrition may empty from the stomach more easily than solid foods.
2. Blood Glucose Monitoring
Frequent monitoring is essential to detect Blood Sugar Swings early. CGM systems can provide real-time alerts.
3. Adjusting Insulin Timing
Doctors may recommend:
- Taking insulin after meals instead of before
- Using rapid-acting insulin
- Splitting insulin doses
These adjustments help better match insulin action with delayed digestion.
4. Medications for Gastroparesis
Prokinetic medications may stimulate stomach contractions and improve emptying.
5. Hydration and Electrolyte Balance
Vomiting can cause dehydration, worsening glucose instability.
Advanced Treatment Options
In severe cases, additional treatments may be necessary:
- Gastric electrical stimulation
- Feeding tubes
- Intravenous nutrition
- Surgical intervention
These options are typically reserved for individuals with severe symptoms and uncontrollable Blood Sugar Swings.
Lifestyle Strategies to Reduce Blood Sugar Swings
Beyond medical treatment, lifestyle modifications can help stabilize glucose levels:
- Regular physical activity (as tolerated)
- Stress management techniques
- Consistent meal timing
- Avoiding alcohol
- Smoking cessation
Stress hormones can significantly impact glucose control, so emotional well-being plays a key role.
The Psychological Impact
Living with both gastroparesis and unpredictable Blood Sugar Swings can be emotionally exhausting. Many patients experience anxiety, depression, or frustration due to the constant need for monitoring and adjustment.
Support groups, counseling, and diabetes education programs can provide valuable coping strategies.
Prevention: Can Blood Sugar Swings Be Avoided?
While gastroparesis may not always be preventable, controlling blood sugar early can reduce nerve damage risk.
Preventive strategies include:
- Maintaining HbA1c within target range
- Regular medical check-ups
- Prompt treatment of digestive symptoms
- Healthy dietary habits
Early intervention can significantly reduce the severity of future Blood Sugar Swings.
When to Seek Medical Help
Immediate medical attention is necessary if you experience:
- Persistent vomiting
- Severe abdominal pain
- Confusion or loss of consciousness
- Extremely high or low blood sugar readings
- Signs of dehydration
These symptoms may indicate a medical emergency.
Long-Term Outlook
With proper management, individuals can successfully control both gastroparesis and Blood Sugar Swings. However, treatment often requires patience and collaboration between:
- Primary care physicians
- Endocrinologists
- Gastroenterologists
- Dietitians
Technology, such as insulin pumps and continuous glucose monitors, has significantly improved outcomes.
Final Thoughts
The relationship between gastroparesis and Blood Sugar Swings highlights the intricate connection between digestive and metabolic health. When the stomach fails to empty properly, blood glucose control becomes unpredictable and challenging.
Understanding this connection empowers patients and healthcare providers to make informed adjustments. Through dietary changes, careful monitoring, medication management, and lifestyle support, it is possible to break the cycle of instability.
While the journey may be complex, proactive care and early intervention can prevent serious complications and improve quality of life. If you are experiencing unexplained Blood Sugar Swings alongside digestive symptoms, seeking medical evaluation may be the first step toward regaining control.