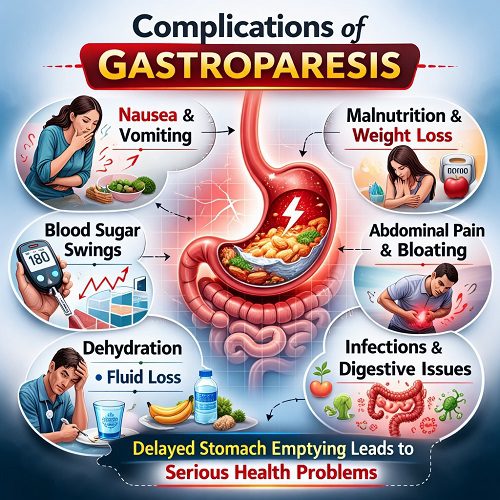
Gastroparesis is a chronic digestive disorder characterized by delayed gastric emptying in the absence of a mechanical obstruction. In simple terms, the stomach takes much longer than normal to move food into the small intestine. This delay can cause a wide range of symptoms, including nausea, vomiting, bloating, early satiety, and abdominal discomfort. While these symptoms can be distressing on their own, the real concern lies in the potential complications that can develop over time.
Understanding the complications of gastroparesis is crucial for patients, caregivers, and healthcare providers alike. Without proper management, this condition can significantly affect nutritional status, blood sugar control, overall health, and quality of life. This article explores the major complications associated with gastroparesis and explains why early diagnosis and consistent treatment are essential.
1. Malnutrition
One of the most serious complications of gastroparesis is malnutrition. Because the stomach empties slowly, patients often feel full after eating only small amounts of food. Persistent nausea and vomiting further reduce appetite and food intake. Over time, this can lead to inadequate consumption of calories, proteins, vitamins, and minerals.
Malnutrition can weaken the immune system, reduce muscle mass, and impair wound healing. In severe cases, patients may require nutritional support such as liquid meal replacements, feeding tubes, or intravenous nutrition (parenteral nutrition). If left untreated, malnutrition can lead to severe weight loss and systemic health decline.
2. Dehydration
Frequent vomiting is common in gastroparesis, especially during flare-ups. Repeated vomiting causes the body to lose fluids and essential electrolytes such as sodium, potassium, and chloride. When fluid intake does not match fluid loss, dehydration occurs.
Symptoms of dehydration may include:
- Dry mouth
- Dizziness or lightheadedness
- Reduced urination
- Fatigue
- Rapid heart rate
Severe dehydration can lead to kidney problems, low blood pressure, and even hospitalization. Maintaining adequate hydration is a key part of managing gastroparesis.
3. Electrolyte Imbalances
Electrolytes are essential for normal nerve and muscle function, including heart rhythm. Persistent vomiting can disrupt electrolyte balance, particularly potassium levels. Low potassium (hypokalemia) can cause muscle weakness, irregular heart rhythms, and in severe cases, life-threatening cardiac complications.
Electrolyte imbalances may not always cause obvious symptoms at first, making regular monitoring important for individuals with chronic vomiting.
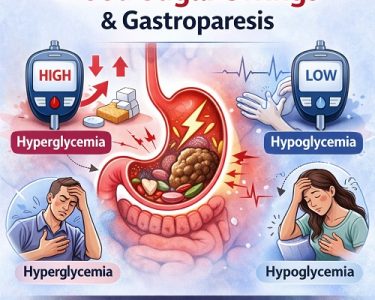
4. Blood Sugar Fluctuations in Diabetic Patients
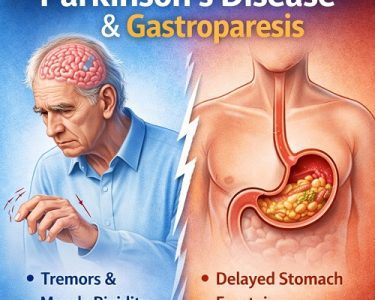
Gastroparesis is commonly associated with diabetes, particularly long-standing type 1 and type 2 diabetes. Damage to the vagus nerve—responsible for controlling stomach muscles—can impair gastric emptying.
In diabetic patients, gastroparesis creates a serious challenge for blood sugar management. Because food leaves the stomach unpredictably, glucose absorption becomes inconsistent. This may result in:
- Sudden spikes in blood sugar (hyperglycemia)
- Unexpected drops in blood sugar (hypoglycemia)
- Difficulty timing insulin doses accurately
Poor blood sugar control can worsen nerve damage, creating a vicious cycle that further aggravates gastroparesis.
5. Bezoar Formation
Another significant complication of gastroparesis is the formation of bezoars. A bezoar is a hardened mass of undigested food that accumulates in the stomach. Because the stomach does not empty properly, food can remain inside long enough to clump together and solidify.
Bezoars can cause:
- Severe nausea and vomiting
- Stomach pain
- Obstruction of the stomach outlet
- Worsening of gastroparesis symptoms
In some cases, bezoars must be removed through endoscopy or, rarely, surgery. Preventing bezoars often requires dietary changes, such as avoiding high-fiber foods that are difficult to digest.
6. Gastroesophageal Reflux Disease (GERD)
Delayed gastric emptying increases pressure within the stomach, which can contribute to acid reflux. When stomach contents flow backward into the esophagus, it causes symptoms such as heartburn, regurgitation, and chest discomfort.
Chronic reflux may lead to complications like:
- Esophagitis (inflammation of the esophagus)
- Esophageal ulcers
- Barrett’s esophagus (a precancerous condition)
Thus, gastroparesis may indirectly increase the risk of long-term esophageal damage.
7. Small Intestinal Bacterial Overgrowth (SIBO)
Stagnant food in the stomach and upper small intestine can create an environment favorable for bacterial overgrowth. When bacteria multiply excessively in the small intestine, it can lead to bloating, gas, diarrhea, and further nutrient malabsorption.
SIBO can worsen nutritional deficiencies and increase gastrointestinal discomfort, compounding the effects of gastroparesis.
8. Weight Loss and Muscle Wasting
Chronic nausea, vomiting, and reduced caloric intake frequently result in unintended weight loss. Over time, this may lead to muscle wasting (loss of lean body mass). Muscle wasting reduces strength, mobility, and overall physical resilience.
Severe weight loss can compromise immune function and increase vulnerability to infections and other illnesses.
9. Psychological and Emotional Complications
Living with a chronic condition like gastroparesis can significantly affect mental health. Persistent symptoms may interfere with social activities, work performance, and daily functioning. Patients often experience:
- Anxiety
- Depression
- Social isolation
- Reduced quality of life
The unpredictability of symptoms—especially nausea and vomiting—can cause constant worry and stress. Psychological distress may further worsen gastrointestinal symptoms, as the gut-brain connection plays a major role in digestive function.
10. Increased Risk of Hospitalization
Severe flare-ups involving uncontrollable vomiting, dehydration, electrolyte imbalance, or nutritional deficiencies often require hospitalization. Repeated hospital admissions can disrupt daily life and increase healthcare costs.
Patients with advanced gastroparesis may need:
- Intravenous fluids
- Electrolyte correction
- Temporary feeding tubes
- Medication adjustments
Frequent hospital stays can also lead to emotional strain and financial burden.
11. Complications from Feeding Tubes or Surgery
In severe cases, medical interventions such as jejunostomy feeding tubes or gastric electrical stimulation devices may be necessary. While these treatments can improve symptoms, they carry potential risks.
Possible complications include:
- Infection at the tube insertion site
- Tube dislodgement
- Mechanical failure of devices
- Surgical complications
Careful monitoring and proper care are required to minimize these risks.
12. Aspiration Pneumonia
Repeated vomiting increases the risk of aspiration, where stomach contents accidentally enter the lungs. This can lead to aspiration pneumonia, a potentially serious lung infection.
Symptoms of aspiration pneumonia may include coughing, shortness of breath, fever, and chest pain. Immediate medical attention is necessary if aspiration is suspected.
13. Worsening of Underlying Conditions
Gastroparesis often coexists with other chronic illnesses such as diabetes, autoimmune disorders, or neurological conditions. Poor nutrition and unstable blood sugar levels may worsen these underlying diseases.
For example:
- Poor glucose control can accelerate diabetic complications.
- Nutrient deficiencies can worsen anemia or immune dysfunction.
- Chronic inflammation may aggravate autoimmune conditions.
Thus, gastroparesis does not exist in isolation; its complications can influence overall systemic health.
14. Impact on Medication Absorption
Delayed gastric emptying can alter how medications are absorbed in the body. Drugs that rely on predictable stomach emptying may become less effective or act unpredictably.
For example:
- Pain medications
- Antibiotics
- Oral contraceptives
- Diabetes medications
Irregular absorption can reduce treatment effectiveness and complicate medical management.
15. Chronic Fatigue
Fatigue is a common but often overlooked complication of gastroparesis. It may result from:
- Malnutrition
- Dehydration
- Anemia
- Poor sleep due to discomfort
- Emotional stress
Chronic fatigue can significantly reduce productivity and impair daily functioning.
Long-Term Outlook and Prevention of Complications
Although gastroparesis can lead to numerous complications, many can be prevented or minimized with proper management. Key strategies include:
- Eating small, frequent meals
- Choosing low-fat, low-fiber foods
- Staying hydrated
- Monitoring blood glucose carefully (for diabetic patients)
- Taking prescribed medications consistently
- Regular follow-ups with healthcare providers
Early intervention is crucial. The sooner complications are identified, the easier they are to manage.
Conclusion
Gastroparesis is more than just delayed stomach emptying—it is a complex condition that can affect nearly every aspect of a person’s health. From malnutrition and dehydration to blood sugar instability and psychological distress, the complications of gastroparesis can be severe and far-reaching.
However, with careful monitoring, dietary adjustments, medical treatment, and lifestyle changes, many of these complications can be prevented or controlled. Patients should work closely with healthcare providers to create a comprehensive management plan tailored to their individual needs.
Raising awareness about the complications of gastroparesis is essential. Understanding the risks empowers patients to seek timely care, adhere to treatment, and ultimately improve their quality of life.