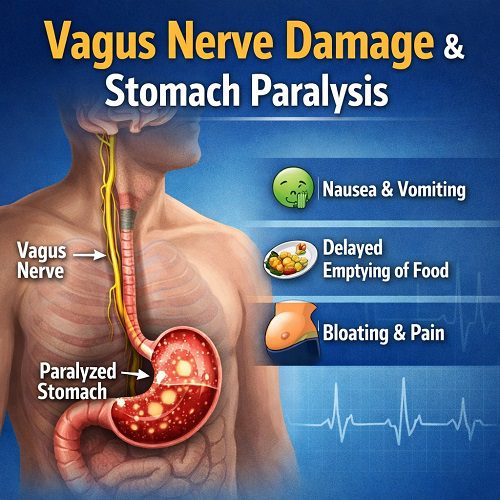
The human body operates through a remarkably intricate communication network between the brain and internal organs. At the center of this system lies the vagus nerve—one of the most important nerves in the body. When this nerve becomes injured or dysfunctional, serious digestive consequences can follow. Among the most significant of these is stomach paralysis, medically known as gastroparesis.
Vagus Nerve Damage is increasingly recognized as a key contributor to digestive disorders that affect millions worldwide. While many people associate digestive symptoms with simple issues like acid reflux or indigestion, fewer understand that the root cause may lie in a malfunctioning nerve. When the vagus nerve fails to properly signal the stomach muscles, food may remain in the stomach far longer than normal, resulting in Stomach Paralysis.
This article explores the anatomy and function of the vagus nerve, the mechanisms of Vagus Nerve Damage, how it leads to Stomach Paralysis, the symptoms, causes, diagnosis, treatment options, and long-term management strategies.
Understanding the Vagus Nerve
The vagus nerve, also known as the tenth cranial nerve (CN X), is one of the longest and most complex nerves in the body. The word “vagus” comes from Latin, meaning “wandering,” an appropriate name because the nerve travels from the brainstem down through the neck and chest into the abdomen, connecting multiple vital organs.
Primary Functions of the Vagus Nerve
The vagus nerve plays a central role in:
- Regulating heart rate
- Controlling breathing
- Stimulating digestive enzyme production
- Coordinating stomach contractions
- Managing swallowing and speech
- Influencing immune and inflammatory responses
Most importantly for digestion, the vagus nerve controls the movement of food from the stomach into the small intestine through coordinated muscle contractions known as peristalsis.
When functioning properly, the vagus nerve sends signals that instruct the stomach muscles to contract rhythmically, grinding food and pushing it forward. When Vagus Nerve Damage occurs, this signaling process is disrupted, which can ultimately lead to Stomach Paralysis.
What Is Vagus Nerve Damage?
Vagus Nerve Damage refers to impairment or dysfunction of the vagus nerve due to injury, disease, inflammation, or degeneration. Because the vagus nerve regulates multiple organs, damage can result in wide-ranging symptoms, including digestive problems, heart irregularities, and autonomic nervous system dysfunction.
How Vagus Nerve Damage Affects Digestion
The digestive system depends heavily on neural communication. The vagus nerve stimulates:
- Gastric acid secretion
- Digestive enzyme release
- Coordinated stomach muscle movement
- Pyloric sphincter relaxation (allowing food to exit the stomach)
When Vagus Nerve Damage interrupts these signals:
- The stomach muscles may weaken or stop contracting.
- Food remains undigested for extended periods.
- Nausea and bloating increase.
- Nutritional absorption becomes impaired.
Over time, this dysfunction can evolve into Stomach Paralysis.
What Is Stomach Paralysis (Gastroparesis)?
Stomach Paralysis, medically known as gastroparesis, is a condition in which the stomach cannot empty food normally despite the absence of a physical blockage.
In individuals with Stomach Paralysis:
- Food may remain in the stomach for hours or even days.
- The stomach fails to contract efficiently.
- Digestion slows dramatically.
The most common underlying cause is Vagus Nerve Damage.
The Link Between Vagus Nerve Damage & Stomach Paralysis
The relationship between Vagus Nerve Damage and Stomach Paralysis is direct and significant.
Step-by-Step Breakdown
- Initial Injury or Dysfunction
The vagus nerve becomes impaired due to diabetes, surgery, infection, or trauma. - Signal Disruption
The brain can no longer properly communicate with stomach muscles. - Loss of Motility
Gastric muscles fail to contract normally. - Delayed Gastric Emptying
Food accumulates in the stomach. - Development of Symptoms
Nausea, vomiting, bloating, and early satiety begin. - Progression to Stomach Paralysis
Chronic dysfunction leads to gastroparesis.
Without proper neural signaling, even a structurally healthy stomach cannot function correctly.
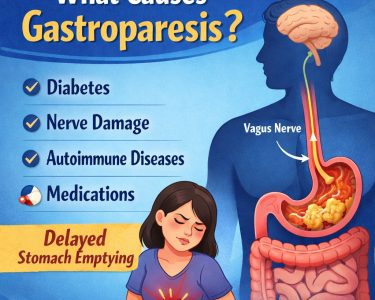
Causes of Vagus Nerve Damage
Several conditions can cause Vagus Nerve Damage, increasing the risk of Stomach Paralysis.
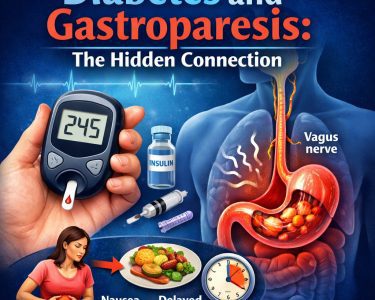
1. Diabetes (Most Common Cause)
Chronic high blood sugar damages nerves throughout the body, including the vagus nerve. This is called diabetic neuropathy.
Over time:
- Elevated glucose damages small blood vessels.
- Nerve fibers deteriorate.
- Digestive motility declines.
Diabetes accounts for a large percentage of Stomach Paralysis cases.
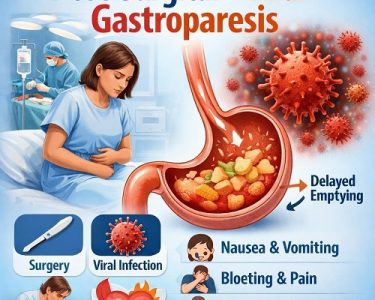
2. Surgical Complications
Surgeries involving the stomach, esophagus, or chest—such as bariatric surgery or anti-reflux procedures—can accidentally injure the vagus nerve.
3. Viral Infections
Some viral infections can temporarily or permanently damage nerve tissue, leading to post-viral gastroparesis.
4. Neurological Disorders
Conditions such as:
- Parkinson’s disease
- Multiple sclerosis
- Stroke
can impair autonomic nervous system function, including the vagus nerve.
5. Autoimmune Conditions
Certain autoimmune disorders attack nerve tissues, potentially causing Vagus Nerve Damage.
6. Trauma
Severe neck or chest injuries may directly impact the nerve.
Symptoms of Vagus Nerve Damage
Because the vagus nerve influences multiple organs, symptoms may extend beyond digestion.
Digestive Symptoms
- Nausea
- Vomiting undigested food
- Bloating
- Abdominal pain
- Early fullness
- Acid reflux
- Constipation
Cardiovascular Symptoms
- Irregular heartbeat
- Fainting spells
General Autonomic Symptoms
- Fatigue
- Dizziness
- Blood pressure fluctuations
When symptoms are primarily digestive and chronic, Stomach Paralysis is often suspected.
Symptoms of Stomach Paralysis
The hallmark of Stomach Paralysis is delayed gastric emptying.
Common symptoms include:
- Persistent nausea
- Vomiting several hours after eating
- Feeling full after small meals
- Loss of appetite
- Weight loss
- Malnutrition
- Dehydration
In severe cases, undigested food may harden into masses called bezoars, which can cause blockages.
Diagnosis
Diagnosing Vagus Nerve Damage and Stomach Paralysis requires a thorough evaluation.
Medical History & Physical Exam
Doctors assess:
- Symptom patterns
- History of diabetes
- Surgical history
- Neurological conditions
Gastric Emptying Study
This is the gold standard test for Stomach Paralysis. The patient eats a small meal containing a harmless radioactive marker. Imaging tracks how quickly food leaves the stomach.
Delayed emptying confirms gastroparesis.
Endoscopy
Used to rule out mechanical blockages.
Autonomic Testing
Specialized tests evaluate vagus nerve function.
Complications of Untreated Vagus Nerve Damage
If Vagus Nerve Damage is not addressed, Stomach Paralysis may worsen.
Potential complications include:
- Severe malnutrition
- Dehydration
- Blood sugar instability
- Bacterial overgrowth
- Intestinal blockages
- Reduced quality of life
Diabetic patients may experience particularly unstable glucose levels because food absorption becomes unpredictable.
Treatment Options
Treatment focuses on symptom relief, improving gastric motility, and addressing underlying causes of Vagus Nerve Damage.
1. Dietary Changes
Diet is the cornerstone of management.
Recommended strategies:
- Small, frequent meals
- Low-fat foods
- Low-fiber foods
- Soft or liquid meals
- Avoid carbonated drinks
Liquids empty from the stomach more easily than solids.
2. Blood Sugar Control (For Diabetics)
Tight glucose control helps prevent further Vagus Nerve Damage.
3. Medications
Doctors may prescribe:
- Prokinetic agents (stimulate stomach contractions)
- Antiemetics (reduce nausea)
- Acid-reducing medications
4. Gastric Electrical Stimulation
In severe cases, a small device may be implanted to stimulate stomach muscles.
5. Feeding Tubes
In advanced Stomach Paralysis, temporary or permanent feeding tubes may be required.
6. Vagus Nerve Stimulation Therapy
Emerging therapies explore targeted stimulation to restore nerve function.
Can Vagus Nerve Damage Be Reversed?
Whether Vagus Nerve Damage can be reversed depends on the cause.
- Diabetic neuropathy: Often partially reversible with strict glucose control.
- Post-surgical damage: May be permanent.
- Post-viral damage: Sometimes improves over months.
- Autoimmune causes: May respond to immunotherapy.
Early intervention improves outcomes.
Lifestyle Strategies to Support Vagus Nerve Health
Certain practices may support vagal tone and autonomic balance:
- Deep diaphragmatic breathing
- Meditation
- Yoga
- Cold exposure therapy
- Regular exercise
- Adequate sleep
While these strategies do not cure Stomach Paralysis, they may improve overall autonomic regulation.
Psychological Impact
Chronic digestive conditions significantly affect mental health.
Patients with Vagus Nerve Damage and Stomach Paralysis often experience:
- Anxiety
- Depression
- Social isolation
- Fear of eating
Integrated care including mental health support is essential.
Emerging Research
Research into Vagus Nerve Damage and gastroparesis continues to evolve.
Areas of investigation include:
- Regenerative nerve therapies
- Stem cell research
- Advanced neuromodulation devices
- Microbiome-based interventions
- Personalized medicine approaches
Greater understanding of the gut-brain axis is opening new treatment pathways.
Living With Stomach Paralysis
Managing Stomach Paralysis requires ongoing adjustments.
Daily Management Tips
- Keep a food diary
- Stay hydrated
- Eat slowly
- Sit upright after meals
- Avoid lying down for 2 hours after eating
- Monitor blood sugar regularly
Support groups can provide valuable emotional and practical assistance.
When to Seek Medical Help
Immediate medical attention is needed if:
- Vomiting is persistent
- There is significant weight loss
- Severe abdominal pain occurs
- Signs of dehydration appear
- Blood sugar becomes dangerously unstable
Early treatment can prevent severe complications.
Prevention
While not all causes are preventable, risk can be reduced by:
- Maintaining healthy blood sugar levels
- Managing autoimmune conditions
- Avoiding unnecessary surgeries
- Seeking early treatment for neurological symptoms
Preventing Vagus Nerve Damage significantly lowers the risk of Stomach Paralysis.
Conclusion
Vagus Nerve Damage is a serious condition that can profoundly disrupt digestive health. Because the vagus nerve plays a central role in coordinating stomach motility, its impairment can directly lead to Stomach Paralysis, or gastroparesis.
Understanding the connection between these two conditions is crucial for early diagnosis and effective management. While there is currently no universal cure, a combination of dietary strategies, medication, medical therapies, and lifestyle modifications can significantly improve quality of life.
As research advances, hope continues to grow for more targeted and regenerative treatments aimed at restoring nerve function and reversing digestive paralysis. Early recognition, proactive care, and comprehensive management remain the keys to controlling symptoms and preventing complications.
If you suspect Vagus Nerve Damage or experience symptoms of Stomach Paralysis, consult a healthcare professional for proper evaluation and personalized treatment.