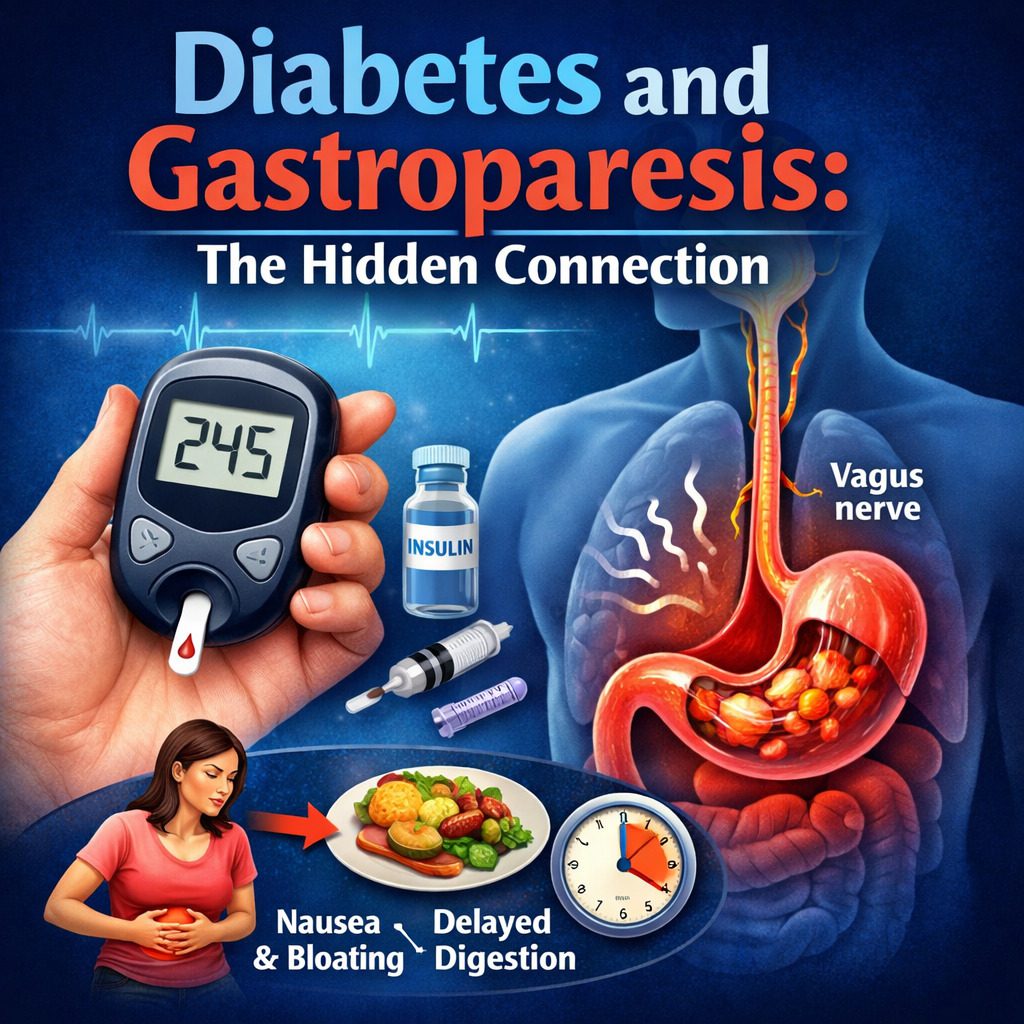
Living with diabetes means constantly balancing blood sugar levels, diet, medication, and lifestyle. Yet beyond the well-known complications such as neuropathy, kidney disease, and vision problems, there is another condition that often goes unnoticed until it significantly disrupts daily life: gastroparesis. The link between Diabetes and Gastroparesis is powerful but frequently misunderstood. For many people, digestive symptoms may be the first sign that blood sugar has been affecting the body in deeper ways than expected.
This article explores the hidden connection between Diabetes and Gastroparesis, explaining how they are linked, why the condition develops, its symptoms, diagnosis, management strategies, and what patients can do to regain control of their digestive health.
Understanding Diabetes
Diabetes mellitus is a chronic metabolic condition characterized by elevated blood glucose levels. The two most common types are:
- Type 1 diabetes – an autoimmune condition in which the body does not produce insulin.
- Type 2 diabetes – a condition involving insulin resistance and often reduced insulin production.
Over time, persistently high blood sugar can damage nerves, blood vessels, and various organs. While many people are aware of complications such as diabetic neuropathy affecting the hands and feet, fewer realize that the digestive system can also be impacted.
This is where the connection between Diabetes and Gastroparesis becomes especially important.
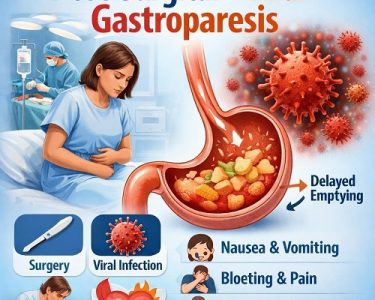
What Is Gastroparesis?
Gastroparesis, sometimes called “delayed gastric emptying,” is a condition in which the stomach takes too long to empty its contents into the small intestine. Unlike a blockage or obstruction, gastroparesis occurs because the stomach muscles do not function properly.
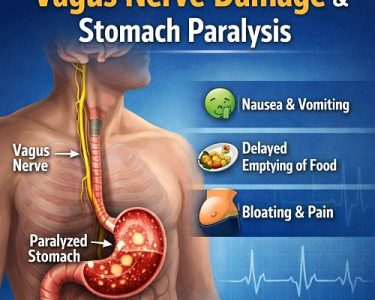
Normally, after eating, the stomach muscles contract to grind food and push it forward into the digestive tract. This process is controlled by the vagus nerve. When this nerve is damaged, the stomach’s ability to contract effectively is reduced.
The result? Food stays in the stomach longer than it should, leading to uncomfortable and sometimes severe digestive symptoms.
The Link Between Diabetes and Gastroparesis
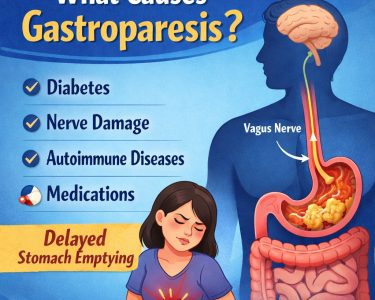
The relationship between Diabetes and Gastroparesis centers on nerve damage. Chronic high blood sugar can damage the vagus nerve, which controls stomach muscle contractions. This type of nerve damage is known as autonomic neuropathy.
When the vagus nerve is impaired:
- Stomach muscles do not contract normally.
- Food remains in the stomach for extended periods.
- Blood sugar levels become more difficult to predict.
In fact, Diabetes and Gastroparesis create a two-way problem. Poorly controlled diabetes can cause gastroparesis, and gastroparesis can make blood sugar control significantly more challenging.
Why Gastroparesis Makes Blood Sugar Harder to Control
One of the most frustrating aspects of Diabetes and Gastroparesis is how each condition worsens the other.
Here’s how it happens:
- Delayed food absorption – When food sits in the stomach, glucose enters the bloodstream unpredictably.
- Insulin timing problems – Insulin may be taken before meals, but if digestion is delayed, insulin may peak before glucose enters the blood.
- Unexpected blood sugar spikes – When food finally moves into the intestine, blood sugar can rise suddenly.
This unpredictable pattern increases the risk of:
- Hypoglycemia (low blood sugar)
- Hyperglycemia (high blood sugar)
- Greater difficulty maintaining stable glucose levels
Managing Diabetes and Gastroparesis together often requires adjustments in insulin timing, medication, and meal planning.
Symptoms of Gastroparesis in People with Diabetes
The symptoms of gastroparesis can vary from mild to severe. In the context of Diabetes and Gastroparesis, symptoms may include:
- Nausea
- Vomiting undigested food
- Feeling full quickly (early satiety)
- Bloating
- Abdominal pain
- Loss of appetite
- Weight loss
- Acid reflux
- Fluctuating blood sugar levels
Some individuals may not experience dramatic digestive symptoms but notice unexplained swings in glucose readings. For these patients, gastroparesis may initially be suspected because of erratic diabetes control rather than digestive complaints.
Who Is at Risk?
While gastroparesis can affect anyone, certain groups have a higher risk, particularly in relation to Diabetes and Gastroparesis:
- Individuals with long-standing diabetes (more than 10 years)
- Those with poorly controlled blood sugar
- People with other forms of diabetic neuropathy
- Women (gastroparesis is more common in females)
- Individuals with autoimmune conditions
Both Type 1 and Type 2 diabetes can lead to gastroparesis, though it is often more common in people with Type 1 diabetes due to longer disease duration.
How Gastroparesis Is Diagnosed
Diagnosing gastroparesis involves ruling out other causes of similar symptoms, such as ulcers or blockages. Doctors may use several tests, including:
1. Gastric Emptying Study
This is the most common test. The patient eats a meal containing a small amount of radioactive material, and imaging tracks how quickly the food leaves the stomach.
2. Upper Endoscopy
Used to rule out structural problems in the stomach.
3. Smart Pill (Wireless Motility Capsule)
A small capsule is swallowed to measure digestive transit times.
When evaluating Diabetes and Gastroparesis, doctors also carefully review blood sugar patterns to look for unexplained fluctuations.
Complications of Diabetes and Gastroparesis
If left untreated, the combination of Diabetes and Gastroparesis can lead to serious complications:
- Severe dehydration from vomiting
- Malnutrition
- Bezoars (hardened masses of undigested food)
- Increased hospitalizations
- Poor overall diabetes control
- Reduced quality of life
The unpredictability of digestion can also cause emotional distress, anxiety around eating, and frustration with diabetes management.
Treatment Strategies for Diabetes and Gastroparesis
There is no complete cure for gastroparesis, but symptoms can be managed effectively with a comprehensive plan. Managing Diabetes and Gastroparesis requires a dual approach—addressing both blood sugar control and digestive function.
1. Optimizing Blood Sugar Control
Better glucose control can prevent further nerve damage and may improve symptoms. Strategies include:
- Continuous glucose monitoring (CGM)
- Insulin pump therapy
- Adjusting insulin timing (taking insulin after meals instead of before)
- Frequent blood sugar checks
Stabilizing blood sugar is foundational in treating Diabetes and Gastroparesis.
2. Dietary Modifications
Diet plays a critical role in symptom management. Recommendations often include:
- Eating smaller, more frequent meals
- Chewing food thoroughly
- Reducing high-fat foods
- Limiting high-fiber foods (which are harder to digest)
- Choosing soft or liquid foods
- Avoiding carbonated beverages
Liquid nutrition may empty the stomach more easily than solid food, making smoothies or soups helpful options.
3. Medications
Several medications may help stimulate stomach emptying or control nausea:
- Prokinetic agents (to stimulate stomach movement)
- Antiemetic medications (to reduce nausea and vomiting)
Medication choices must be carefully considered in patients with Diabetes and Gastroparesis, as some drugs may affect blood sugar levels.
4. Advanced Therapies
In severe cases, additional treatments may be considered:
- Gastric electrical stimulation
- Feeding tubes (for severe malnutrition)
- Surgical interventions in rare situations
These options are typically reserved for individuals whose symptoms do not improve with conservative treatment.
The Emotional Impact of Diabetes and Gastroparesis
Beyond physical symptoms, the combination of Diabetes and Gastroparesis can take a significant emotional toll. Constant nausea, unpredictable blood sugar swings, and dietary restrictions can lead to:
- Anxiety about eating
- Depression
- Social withdrawal
- Fear of hypoglycemia
It’s essential for patients to receive not only medical care but also emotional support. Working with diabetes educators, dietitians, and mental health professionals can make a meaningful difference.
Prevention: Can Gastroparesis Be Avoided?
While not all cases are preventable, maintaining tight blood sugar control significantly reduces the risk. The strongest protective factor against developing complications related to Diabetes and Gastroparesis is consistent glucose management.
Preventive strategies include:
- Regular HbA1c monitoring
- Routine diabetes check-ups
- Early reporting of digestive symptoms
- Healthy eating habits
- Regular physical activity
Early detection allows for earlier intervention, which may slow progression.
Living Well with Diabetes and Gastroparesis
Although challenging, it is possible to live well with Diabetes and Gastroparesis. Key strategies include:
- Partnering closely with healthcare providers
- Keeping detailed food and glucose logs
- Adjusting insulin timing under medical guidance
- Staying hydrated
- Practicing stress management
Each person’s experience is unique, and treatment must be individualized. Patience and persistence are critical.
The Importance of Awareness
One of the biggest challenges surrounding Diabetes and Gastroparesis is lack of awareness. Many patients assume digestive symptoms are unrelated or temporary. Healthcare providers may also focus more heavily on other diabetic complications.
Increasing awareness helps ensure:
- Earlier diagnosis
- Better blood sugar management
- Reduced complications
- Improved quality of life
Understanding the hidden connection empowers patients to advocate for themselves.
Final Thoughts
The relationship between Diabetes and Gastroparesis is complex, bidirectional, and often overlooked. Chronic high blood sugar can damage the vagus nerve, leading to delayed gastric emptying. In turn, delayed digestion makes blood sugar control more unpredictable and difficult.
Recognizing the symptoms early, optimizing glucose management, modifying diet, and working with healthcare professionals can significantly improve outcomes. While there may not be a cure, proactive management can dramatically enhance comfort, stability, and overall well-being.
If you or someone you know has diabetes and experiences persistent digestive symptoms, it may be time to explore the possibility of gastroparesis. Understanding the connection between Diabetes and Gastroparesis is the first step toward regaining control and improving quality of life.