When people think of bullous pemphigoid, they often imagine painful blisters on the skin. But did you know that this autoimmune condition can also affect the inside of your mouth? Understanding the difference between bullous pemphigoid oral and skin manifestations is crucial for accurate diagnosis and effective treatment.
In this comprehensive guide, we’ll explore how bullous pemphigoid impacts both the skin and the oral cavity, what symptoms to look for, how they differ, and why these distinctions matter for managing your condition. We’ll also touch on important care routines and treatments that help you live more comfortably with this chronic disorder.
Before we dive deeper, it’s also essential to recognize that patients often wonder about related aspects of living with the condition—such as can you shower with bullous pemphigoid safely—since maintaining skin hygiene is a big part of daily management.
Understanding Bullous Pemphigoid: An Overview
Bullous pemphigoid is an autoimmune blistering disease that causes the immune system to mistakenly attack the proteins that hold the skin’s layers together. This leads to large, fluid-filled blisters on the skin, often accompanied by itching and redness.
Most commonly, it affects older adults, but it can appear in younger individuals too. The condition typically begins with red, itchy patches that later develop into tense blisters. These blisters usually appear on the lower abdomen, inner thighs, armpits, and sometimes the arms or legs.
However, bullous pemphigoid can also affect mucous membranes, including the mouth, gums, and even the throat. This form is known as bullous pemphigoid oral, and it can make eating, brushing, and speaking painful.
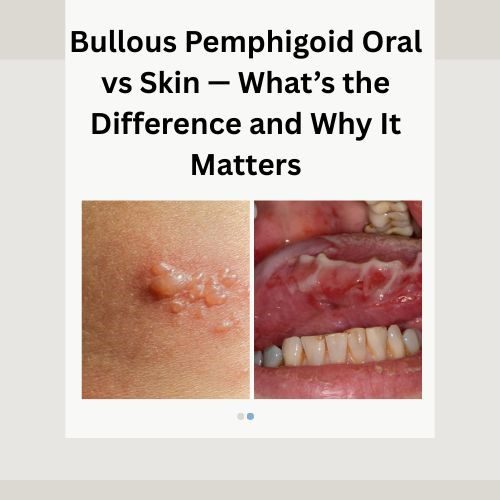
Bullous Pemphigoid Oral vs Skin — Key Differences
The main difference between bullous pemphigoid affecting the skin and that affecting the oral cavity lies in the location, symptoms, and healing process. Let’s explore these differences in detail.
Location of Blisters
- Skin Bullous Pemphigoid:
Blisters appear mainly on areas of the body that experience friction or movement — such as the abdomen, arms, legs, or groin. - Bullous Pemphigoid Oral:
Blisters form inside the mouth, gums, inner cheeks, and sometimes on the tongue. They can also appear in the throat or esophagus, making swallowing difficult.
Appearance and Symptoms
On the skin, blisters are tense, filled with fluid, and rarely rupture on their own. They often heal without scarring unless secondary infection occurs.
In contrast, bullous pemphigoid oral cavity blisters are more fragile. They tend to break easily, leaving behind raw, painful ulcers that may resemble canker sores. These lesions can make it hard to eat, drink, or maintain oral hygiene.
Patients with bullous pemphigoid mouth symptoms often experience burning sensations or bleeding gums, particularly when brushing teeth or eating acidic foods.
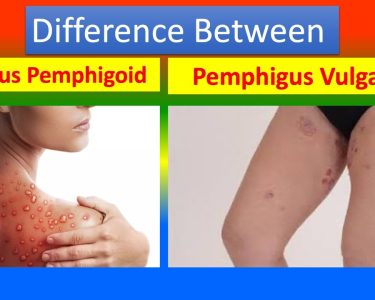
Diagnosis
Diagnosing bullous pemphigoid can be challenging because oral lesions can mimic other conditions such as lichen planus or pemphigus vulgaris. Dermatologists and oral pathologists often rely on a biopsy and direct immunofluorescence testing to confirm the diagnosis.
When only the oral cavity is affected, the disease might initially be misdiagnosed as another mucosal disorder. Therefore, recognizing the difference between bullous pemphigoid in oral cavity and skin manifestations helps ensure appropriate treatment.
Healing and Recovery
Skin blisters may heal in a few weeks if managed well, while oral lesions take longer due to constant moisture and movement in the mouth. Eating and talking can aggravate ulcers, delaying healing and increasing the risk of infection.
Moreover, oral lesions require specific oral hygiene routines, including non-alcoholic mouth rinses and gentle brushing with soft-bristled toothbrushes.
Why the Difference Matters
Understanding whether bullous pemphigoid affects your skin or mouth—or both—is important because the treatment and management strategies differ.
For skin lesions, topical corticosteroids or oral medications may be sufficient. However, oral involvement might require additional care such as medicated mouth rinses, numbing gels, or dietary adjustments.
When blisters occur in the mouth, maintaining nutrition can become a challenge. Patients are often advised to consume soft, non-spicy foods and avoid acidic items that may irritate the mucosa. In this context, doctors frequently emphasize foods to avoid with bullous pemphigoid to minimize flare-ups and discomfort.
What Causes Oral Bullous Pemphigoid?
The exact cause remains unclear, but it is widely understood to be an autoimmune reaction. The body’s immune system mistakenly targets proteins that connect the outer and inner layers of the skin and mucous membranes, leading to blister formation.
Certain medications, infections, or underlying conditions may trigger or worsen the immune response. Stress and inflammation can also contribute to flare-ups.
Both oral and skin manifestations share the same autoimmune mechanism but differ in presentation and management strategies.
Common Triggers for Oral Flare-Ups
Even though bullous pemphigoid is not contagious, flare-ups can occur when the immune system becomes overactive. Common triggers include:
- High levels of stress or emotional strain
- Certain antibiotics, diuretics, or pain medications
- Trauma to the mouth (from dental procedures or sharp foods)
- Inflammatory foods such as citrus fruits, spicy dishes, or processed foods
- Hormonal changes and infections
Managing these triggers can significantly reduce the severity and frequency of flare-ups.
Treating Oral vs Skin Bullous Pemphigoid
Treatment for bullous pemphigoid depends on the severity and extent of the condition. Both oral and skin forms require medical supervision, but oral lesions often need additional interventions for comfort and hygiene.
For Skin Bullous Pemphigoid:
- Topical corticosteroids or oral steroids
- Immunosuppressive drugs (azathioprine, methotrexate)
- Antibiotics for secondary infections
- Gentle skincare routines and emollients
For Oral Bullous Pemphigoid:
- Medicated mouth rinses (chlorhexidine or steroid-based)
- Topical gels for pain relief
- Avoiding spicy or acidic foods
- Soft diets to prevent trauma
- Oral corticosteroids or immunosuppressants in severe cases
Patients exploring alternative healing approaches often look into herbal treatment for bullous pemphigoid, which may include soothing agents like aloe vera or chamomile. However, these should always be discussed with a healthcare professional before use.
The Role of Lifestyle and Oral Hygiene
Maintaining proper oral hygiene is critical in managing bullous pemphigoid oral lesions. Use a soft toothbrush and fluoride-free toothpaste to minimize irritation. Avoid mouthwashes containing alcohol or menthol, as they can cause stinging and dryness.
It’s also important to keep the mouth hydrated. Drinking water frequently and using saliva substitutes can help prevent discomfort caused by dry mouth.
Lifestyle changes like quitting smoking, reducing stress, and eating anti-inflammatory foods can improve your overall skin and oral health. These small steps contribute to faster healing and fewer recurrences.
Natural Remedies and Supportive Care
In addition to medical treatments, some individuals turn to the real Story behind bullous pemphigoid natural remedies to complement conventional care. Natural remedies such as honey, turmeric, and aloe vera are known for their anti-inflammatory properties.
However, it’s vital to approach these options cautiously. Always consult your dermatologist or oral specialist before trying any herbal or natural product, as not all remedies are suitable for open lesions or sensitive mucous membranes.
Can Bullous Pemphigoid in the Mouth Heal Completely?
With proper treatment, oral lesions can heal completely, but remission times vary among patients. Some may experience recurrent flare-ups, while others enjoy long periods without symptoms.
Sticking to prescribed treatments, maintaining good oral care, and following a healthy lifestyle can help keep symptoms under control.
For those exploring gentle complementary approaches, natural treatments for bullous pemphigoid may provide supportive benefits, but should never replace professional medical guidance.
When to Seek Medical Help
If you notice persistent sores in your mouth that don’t heal, or if your skin blisters worsen despite treatment, it’s essential to see a dermatologist or oral medicine specialist. Prompt diagnosis ensures effective management and prevents complications such as infection or scarring.
Persistent pain, bleeding, or difficulty swallowing should always be evaluated to rule out other oral diseases.
The Importance of Ongoing Care
Managing bullous pemphigoid is not a one-time effort—it’s a long-term journey. Regular follow-ups, proper medication use, and awareness of triggers are essential for keeping flare-ups under control.
Your doctor might also adjust your medications over time to reduce side effects while maintaining stability. Comprehensive care often involves dermatologists, dentists, and immunologists working together for your well-being.
As patients explore different options, many also research treatment options you need to know, ensuring they stay informed about both traditional and emerging therapies.
The Connection Between Skin and Mouth Involvement
In some cases, skin lesions may appear first, followed by oral involvement weeks or months later. For others, mouth lesions may precede skin blisters. Recognizing these patterns helps doctors predict disease progression and tailor treatment accordingly.
While oral lesions can be more painful, skin involvement often causes itching and irritation. Addressing both aspects is key to improving quality of life and long-term outcomes.
Living Comfortably with Bullous Pemphigoid
Adapting to life with bullous pemphigoid involves more than medication—it’s about lifestyle, emotional health, and self-care. Being mindful of triggers, maintaining proper hygiene, and eating a balanced diet all contribute to comfort and healing.
Support groups and counseling can also provide emotional relief, helping you connect with others who understand your journey.
For those interested in holistic care, learning about bullous pemphigoid natural treatment can offer complementary ideas, but always under professional supervision to avoid complications.
Final Thoughts
Understanding the difference between bullous pemphigoid oral and skin forms is essential for effective care and recovery. Both can be managed successfully with the right combination of medical treatment, lifestyle adjustments, and ongoing support.
Whether you’re dealing with oral ulcers or skin blisters, patience and proper care are vital. Keep in touch with your healthcare provider, follow prescribed routines, and explore safe, gentle ways to protect and soothe your skin and mouth.