Introduction: Understanding Achalasia Type II
Achalasia Type II is a rare but serious esophageal disorder that affects how food and liquids pass from the esophagus into the stomach. It belongs to a broader category known as achalasia, a motility disorder where the lower esophageal sphincter (LES) — the muscle that opens to let food enter the stomach — fails to relax properly. This causes a buildup of food in the esophagus, leading to symptoms such as difficulty swallowing, chest pain, regurgitation, and sometimes unintentional weight loss.
While all forms of achalasia share similar core characteristics, Achalasia Type II has distinct features that influence both its diagnosis and treatment options. In recent years, medical research has made significant progress in understanding this condition, leading to innovative therapies and minimally invasive procedures that offer long-term relief for patients.
What patients should know about Achalasia Type II, including how it differs from other subtypes, the latest treatment breakthroughs, and what the future may hold for managing this challenging condition.
What Is Achalasia Type II?
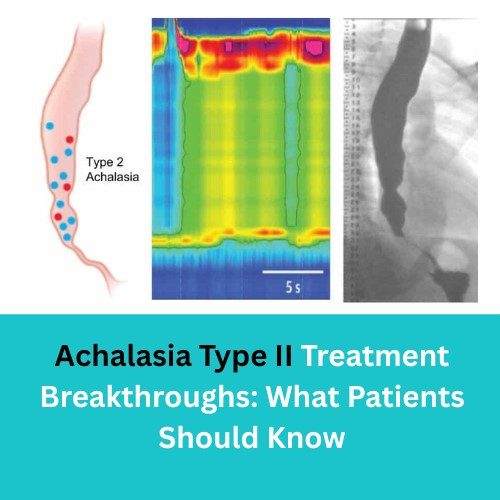
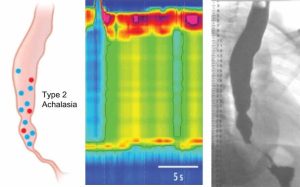
Achalasia is divided into three types based on high-resolution esophageal manometry (HRM) results — a test that measures pressure changes in the esophagus.
- Type I (Classic Achalasia): Minimal esophageal pressure and no peristalsis (muscle contractions).
- Type II: Panesophageal pressurization, meaning the entire esophagus contracts simultaneously instead of in a wave-like motion.
- Type III (Spastic Achalasia): Characterized by spastic, uncoordinated contractions of the esophagus.
Achalasia Type II is the most common and often the most responsive to treatment. The esophagus generates a uniform pressure, but the LES fails to relax, causing food to stagnate. Despite this, Type II tends to have the best prognosis because the esophageal body still exhibits some ability to generate pressure, allowing certain procedures to be more effective compared to other subtypes.
Common Symptoms of Achalasia Type II
Patients with Achalasia Type II typically experience the following symptoms:
- Dysphagia (difficulty swallowing) — for both solids and liquids
- Regurgitation — food or liquid coming back up after swallowing
- Chest pain or pressure — often mistaken for cardiac issues
- Heartburn-like sensations — though not related to acid reflux
- Weight loss — due to poor food intake or malnutrition
- Nocturnal coughing or aspiration — when regurgitated food enters the airway during sleep
Since these symptoms overlap with conditions like gastroesophageal reflux disease (GERD), diagnosis often requires specialized testing.
Diagnosis: How Achalasia Type II Is Identified
Accurate diagnosis is essential for successful treatment. The following tests are commonly used:
1. High-Resolution Manometry (HRM)
This is the gold standard for diagnosing Achalasia Type II. HRM measures the pressure patterns of esophageal muscles and identifies panesophageal pressurization — a hallmark of Type II achalasia.
2. Barium Swallow (Esophagram)
In this imaging test, patients swallow a barium solution that coats the esophagus, allowing doctors to visualize its shape and function on X-ray. It often shows a “bird’s beak” narrowing at the LES.
3. Upper Endoscopy (EGD)
This allows direct visualization of the esophagus and stomach to rule out other causes like strictures, tumors, or inflammation.
Once Type II is confirmed, the next step is determining the most effective treatment strategy — a process that has evolved significantly in recent years.
Traditional Treatments for Achalasia Type II
For decades, the goal of achalasia treatment has been to relieve LES pressure and improve swallowing. Because the underlying nerve damage cannot be reversed, therapies focus on mechanical or surgical interventions.
1. Pneumatic Dilation
This involves inserting a balloon into the LES and inflating it to stretch and weaken the muscle. It’s effective for many patients, particularly those with Type II achalasia, but there’s a risk of perforation and recurrence over time.
2. Heller Myotomy (Laparoscopic Surgery)
A surgical procedure that cuts the LES muscle fibers to allow food to pass more easily. When combined with an anti-reflux procedure (fundoplication), it offers durable relief.
3. Botulinum Toxin (Botox) Injection
Botox injections can temporarily relax the LES muscle. It’s usually reserved for patients who are not candidates for surgery or dilation, as its effects last only a few months.
While these conventional treatments remain effective for many, the past decade has seen remarkable innovations that are reshaping how Achalasia Type II is managed.
Breakthrough Treatments for Achalasia Type II
1. Peroral Endoscopic Myotomy (POEM): A Minimally Invasive Revolution
One of the most significant breakthroughs in recent years is Peroral Endoscopic Myotomy (POEM). This cutting-edge, incisionless procedure uses an endoscope inserted through the mouth to access and cut the LES muscle internally.
How POEM Works:
- The doctor makes a small incision in the esophageal lining.
- The endoscope tunnels through the esophagus to reach the LES.
- The muscle is carefully cut to relieve pressure.
- The entry site is closed with clips — no external incision required.
Advantages:
- Minimally invasive with shorter recovery times.
- High success rate — studies show >90% symptom improvement in Achalasia Type II patients.
- Effective even for patients who have failed other treatments.
Limitations:
- Requires specialized expertise and equipment.
- May increase the risk of post-procedure acid reflux (GERD).
Why It’s a Game Changer:
POEM has quickly become the gold standard for Achalasia Type II in many medical centers worldwide due to its durability and safety.
2. EndoFLIP Technology: Precision in Diagnosis and Monitoring
Another breakthrough aiding both diagnosis and treatment optimization is EndoFLIP (Endolumenal Functional Lumen Imaging Probe). This tool measures the esophagus’s geometry and distensibility (ability to stretch) in real-time during procedures like POEM or dilation.
Benefits:
- Provides accurate feedback during surgery.
- Helps tailor treatment intensity to each patient’s needs.
- May reduce the risk of overtreatment or incomplete myotomy.
By integrating EndoFLIP data, doctors can personalize Achalasia Type II management and predict long-term outcomes more accurately.
3. Novel Pharmacological Research
While surgery and endoscopic techniques dominate treatment, researchers are investigating medications that could help improve esophageal motility or LES relaxation.
Promising agents under study include:
- Nitric oxide donors and calcium channel blockers, which can lower LES pressure.
- Sildenafil (Viagra), which has shown some LES-relaxing effects.
- Gene-targeted therapies that aim to restore nerve signaling to the esophagus (still experimental).
Although these treatments are in early stages, they offer hope for non-invasive management of Achalasia Type II in the future.
4. Robotic-Assisted Heller Myotomy
The integration of robotics into traditional laparoscopic myotomy has enhanced surgical precision and safety. Robotic Heller Myotomy allows finer control and better visualization of delicate esophageal tissues.
Benefits:
- Shorter recovery times.
- Reduced post-operative pain.
- Lower complication rates.
For complex or recurrent Achalasia Type II cases, robotic surgery provides an excellent alternative to conventional methods.
Managing Achalasia Type II: Beyond Surgery
While procedural breakthroughs are transforming outcomes, long-term management remains crucial. Successful treatment requires not only relieving obstruction but also maintaining esophageal health and preventing complications.
1. Dietary Modifications
After treatment, patients are often advised to:
- Eat small, frequent meals to prevent esophageal overload.
- Avoid carbonated drinks, which can cause discomfort.
- Chew thoroughly and eat slowly.
- Stay upright for at least 30 minutes after meals.
Soft, moist foods like soups and smoothies are generally easier to swallow during recovery.
2. Lifestyle and Post-Procedure Care
- Sleep with the head elevated to reduce nighttime regurgitation.
- Avoid alcohol and tobacco, which can worsen symptoms.
- Monitor for reflux symptoms — if persistent, proton pump inhibitors (PPIs) may be prescribed.
- Regular follow-up with gastroenterologists to track esophageal function.
Early detection of recurrence or reflux can prevent further complications.
Complications and Long-Term Outlook
Without treatment, Achalasia Type II can lead to serious complications, including:
- Esophageal dilation or sigmoid esophagus (abnormal bending).
- Aspiration pneumonia from food entering the lungs.
- Increased risk of esophageal cancer due to chronic irritation.
However, with modern therapies like POEM or robotic myotomy, most patients enjoy long-term relief and improved quality of life. Studies indicate that Achalasia Type II has the best prognosis among all subtypes, with success rates exceeding 90% when treated appropriately.
Research and Future Directions
Ongoing research continues to uncover exciting possibilities for Achalasia Type II treatment. Some emerging areas include:
1. Regenerative Medicine and Stem Cell Therapy
Scientists are exploring whether stem cells can repair the damaged nerve cells (ganglia) responsible for achalasia. If successful, this could address the root cause rather than just the symptoms.
2. Artificial Intelligence (AI) in Diagnosis
AI-based imaging tools are being developed to analyze manometry patterns and endoscopic data more accurately, enabling faster and more precise classification of achalasia subtypes.
3. Genetic and Immunological Studies
There’s growing evidence that achalasia may involve autoimmune or genetic components. Understanding these mechanisms may pave the way for preventive treatments or personalized therapies.
Patient Perspective: Living with Achalasia Type II
Receiving an Achalasia Type II diagnosis can feel overwhelming, but understanding the condition empowers patients to make informed choices. With the advent of advanced treatments like POEM and EndoFLIP-guided procedures, many patients return to normal eating and living habits within weeks.
Patient testimonials frequently highlight:
- Relief from years of swallowing difficulty.
- Improved nutrition and energy levels.
- Renewed confidence in social eating situations.
Education and support from gastroenterology specialists and patient networks play a vital role in recovery and long-term well-being.
When to Seek Medical Help
If you experience persistent swallowing difficulties, chest discomfort, or regurgitation, it’s important not to ignore the symptoms. Early evaluation by a gastroenterologist can lead to timely diagnosis and better treatment outcomes. Since Achalasia Type II progresses gradually, recognizing symptoms early can prevent irreversible esophageal damage.
Conclusion: A New Era for Achalasia Type II Treatment
The landscape of Achalasia Type II treatment has evolved dramatically in the past decade. From traditional surgical techniques to advanced endoscopic methods like POEM, patients now have access to safer, more effective, and longer-lasting relief options.
What was once a life-altering diagnosis is now a manageable condition, thanks to innovation, technology, and growing medical expertise. While no cure currently reverses the underlying nerve damage, modern interventions can restore swallowing function, improve quality of life, and prevent complications.
As research continues, the future of Achalasia Type II treatment looks brighter than ever — offering hope, healing, and renewed comfort to patients around the world.