Achalasia — a rare but debilitating disorder of the esophagus — causes the lower esophageal sphincter (LES) to fail to relax, leaving people with progressive difficulty swallowing (dysphagia), regurgitation, chest pain, weight loss, and poor quality of life. For decades the main therapeutic options and Achalasia Natural Treatment were pneumatic (balloon) dilation, laparoscopic Heller myotomy (LHM) with partial fundoplication, botulinum toxin injections for short-term relief, and supportive measures. Over the last decade those approaches have steadily evolved. In 2025 a clear clinical shift has taken hold: peroral endoscopic myotomy (POEM) — refined by intra-procedural physiologic guidance and new adjuncts — has emerged as the most important new treatment for achalasia, while innovations such as EndoFLIP-guided myotomy, POEM combined with anti-reflux strategies, and temporary/biodegradable stents are reshaping options for patients who are elderly, frail, or refractory to standard care.
What changed — why 2025 feels like a “breakthrough” year
Three converging advances explain why clinicians and patients are calling the mid-2020s a turning point:
- Robust long-term data and randomized comparisons that confirm POEM’s durable effectiveness in most achalasia patients, placing it on par with or better than traditional LHM for symptom control. Recent multi-center work with longer follow-up strengthened clinicians’ confidence that POEM is not just an experimental procedure but a durable first-line therapy for many patients.
- Physiology-guided personalization using tools like EndoFLIP (endoscopic functional lumen imaging probe) during procedures to measure the esophagogastric junction distensibility in real time. This lets operators tailor the length and depth of the myotomy to the patient’s individual biomechanics, improving outcomes and reducing incomplete myotomy rates. Societies and clinical updates in 2024–2025 increasingly recommend incorporating EndoFLIP data into the procedural plan.
- New adjunct therapies and device innovations — notably POEM-F (POEM plus endoscopic or surgical fundoplication-like anti-reflux steps), robot-assisted techniques for precision, and improved temporary biodegradable stents — offer tailored options for patients at higher reflux risk or those unsuitable for surgery. Reviews in 2025 highlight growing evidence for these adjuncts as pragmatic ways to reduce postoperative GERD and expand choices for refractory cases.
Taken together, these developments don’t represent a single magical drug or device but a step-change in how clinicians choose, perform, and personalize Natural Herbal Treatment for Achalasia— hence the description “New Treatment for Achalasia” in 2025 often refers to this integrated modern approach centered on POEM + physiology guidance.
Understanding POEM: what it is and why it matters
Peroral endoscopic myotomy (POEM) is an endoscopic procedure that mimics the effect of Heller myotomy but is performed entirely from inside the esophagus. A tunnel is created within the esophageal wall and the circular muscle fibers of the LES are cut (myotomy) to relieve outflow obstruction. Because it is done endoluminally there are no abdominal incisions, and recovery is usually faster than for open or laparoscopic surgery.
Why POEM gained traction:
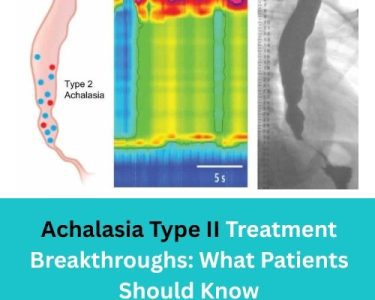
- It allows precise control over the length and orientation of myotomy (useful for type II and type III achalasia where spasm extends proximally).
- Shorter hospital stays and faster return to normal activity in experienced centers.
- Growing multi-center evidence shows comparable or superior symptom control versus LHM at follow-up intervals of 2–5 years in many series.
Clinical outcomes: Recent literature reports clinical success rates after POEM in the 75–98% range depending on follow-up length, disease subtype, and definition of success; however, post-procedural reflux (GERD) is more commonly observed after POEM than after LHM with fundoplication in several series. That tradeoff—excellent dysphagia relief versus higher GERD risk—drives much of the contemporary innovation (see EndoFLIP and anti-reflux adjuncts below).
EndoFLIP and physiology-guided myotomy: personalization is the new standard
EndoFLIP is not a treatment itself but a real-time diagnostic device used during endoscopy. It measures cross-sectional area and intraluminal pressure to calculate a distensibility index (DI) of the esophagogastric junction — essentially how stretchy and open the junction is. Operators can perform an initial measurement, do a staged myotomy, and re-measure until an optimal DI is achieved.
Why that matters:
- Objective feedback: Instead of relying solely on visual cues or symptom reports, EndoFLIP gives numeric targets surgeons can aim for, reducing under- or over-treatment.
- Reduced re-intervention: Early studies and systematic reviews from 2024–2025 suggest EndoFLIP-guided procedures have lower rates of incomplete myotomy and fewer early failures.
- Better tailoring: Some patients need shorter myotomies; others require longer or deeper cuts — EndoFLIP helps decide.
Because of this, major gastroenterology updates in 2025 recommend considering EndoFLIP during myotomy procedures when available, particularly for complex or re-do cases. That is one reason POEM in 2025 is not the same “POEM” of ten years ago — it’s increasingly a physiology-guided procedure.
Tackling reflux: POEM-F and other anti-reflux strategies
A consistent downside to myotomy is gastroesophageal reflux. Laparoscopic Heller myotomy traditionally includes a partial fundoplication to reduce reflux, but POEM lacks that posterior wrap — creating a higher measured reflux incidence in many series.
Responses to this problem in 2025 include:
- POEM-F: combining POEM with endoscopic or minimally invasive anti-reflux maneuvers (various techniques are being piloted, including transoral fundoplication-like approaches or hybrid POEM + surgical fundoplication in selected cases). Early results show promise for lowering post-POEM GERD, but head-to-head long-term data are still emerging.
- Targeted patient selection: using preoperative testing (pH testing, manometry, EndoFLIP) to identify patients at higher baseline reflux risk who might be better served with LHM + fundoplication or POEM with an added anti-reflux plan.
- Medical management: more aggressive and early use of proton pump inhibitors (PPIs) post-procedure along with lifestyle modifications remains routine when GERD occurs.
The bottom line: reflux remains the principal trade-off clinicians must counsel patients about; innovations in 2025 are narrowing the gap but not eliminating the problem entirely.
New device options: stents and biodegradable solutions
For patients who are poor surgical candidates, elderly, or who have failed multiple interventions, temporary self-expanding stents — and more recently biodegradable stents — have been revisited as palliative or bridging treatments. The 2020s saw improved stent designs and small studies indicating acceptable short-term dysphagia relief without the need for repeat endoscopic removal for biodegradable models. However, these are still niche options and not first-line for most patients. Reviews in 2025 emphasize careful patient selection and ongoing monitoring for complications such as migration and tissue overgrowth.
Who is a candidate for the new approaches?
The “new treatment for achalasia” paradigm is not one-size-fits-all. Candidate selection matters:
- Good candidates for POEM + physiology guidance: most people with primary achalasia (types I–III), especially younger or fit patients who prioritize durable dysphagia relief and accept reflux risk or agree to close reflux surveillance.
- Consider LHM + fundoplication: patients with high baseline reflux disease or anatomy where a fundoplication is strongly preferred (some centers still favor LHM in such cases).
- Stents or dilation: considered for elderly frail patients, those refusing surgery, or as temporizing measures. Botulinum toxin injection remains an option for very frail patients or short-term relief.
Shared decision-making with a multidisciplinary team — gastroenterologist, foregut surgeon, and physiologic testing — is essential to choose the right path for any individual.
Risks and side effects to discuss
No procedure is risk-free. Key risks for the new-era treatments include:
- Gastroesophageal reflux disease (GERD): more common after POEM than after LHM with fundoplication in many studies; requires monitoring and sometimes lifelong PPI therapy or additional interventions.
- Perforation, bleeding, infection: uncommon in experienced centers but possible with any endoscopic or surgical myotomy.
- Need for reintervention: a minority of patients may require dilation, re-do myotomy, or other interventions if symptoms recur. EndoFLIP guidance aims to reduce this risk.
Careful pre-procedure counseling and post-procedure surveillance (symptom monitoring, pH testing, and follow-up endoscopy when indicated) are standard.
Practical pathway: diagnosis to treatment in the 2025 era
- Confirm diagnosis: high-resolution manometry is the diagnostic gold standard; complementary tests include timed barium esophagram and upper endoscopy to rule out mechanical obstruction or pseudo-achalasia.
- Physiology mapping: EndoFLIP or impedance planimetry may be used in specialized centers to understand esophagogastric junction mechanics.
- Shared decision-making: discuss POEM (with physiology guidance), LHM + fundoplication, dilation, or other options based on age, comorbidities, reflux risk, and local expertise.
- Procedure at an experienced center: outcomes correlate strongly with operator and center experience. Aim for high-volume centers when possible.
- Follow-up: clinical follow-up, symptom scores (e.g., Eckardt score), and reflux assessment as needed.
What the evidence still needs (and where research is heading)
Despite the enthusiasm, important gaps remain:
- Long-term comparative data beyond 5–10 years for many of these modern approaches is still accruing. Recent randomized data is strong for intermediate-term follow-up, but continued surveillance will refine recommendations. Standardized EndoFLIP protocols: while promising, EndoFLIP lacks universally accepted numeric targets and standard operating procedures; multicenter harmonization is underway.
- Optimal anti-reflux strategy after POEM: multiple approaches (POEM-F, transoral fundoplication, hybrid surgical approaches) are being tested; larger randomized comparisons will help clarify best practice.
- Device innovation for refractory disease: better biodegradable stents and implantable devices may expand options for patients who can’t undergo myotomy. Early reports are promising but require larger trials.
Bottom line: what “New Treatment for Achalasia” means in 2025
If you ask, “What is the new treatment for achalasia?” the most accurate answer in 2025 is: a modern, physiology-guided approach centered on POEM, enhanced by intra-procedural measurement (EndoFLIP), and refined anti-reflux or device adjuncts when needed. This integrated strategy has made achalasia care more precise, more customizable, and in many hands more effective than older paradigms — though trade-offs (especially reflux) still require careful planning.
If you or someone you care for has achalasia: practical advice
- Seek evaluation at a center with experience in achalasia management and access to high-resolution manometry and EndoFLIP when possible.
- Ask your clinician about POEM and whether physiology-guided myotomy is an option for you; discuss reflux risk and anti-reflux plans.
- If you’re elderly, frail, or have significant comorbidities, ask about dilation, botulinum toxin injection, or temporary/biodegradable stents as alternatives.
- Remember that outcomes depend on operator expertise; ask about your center’s experience and complication rates.
Final note and medical disclaimer
This article summarizes evolving medical evidence through 2025 but is not a substitute for personalized medical advice. If you suspect achalasia or are considering treatment changes, please consult a qualified gastroenterologist or foregut surgeon who can interpret your tests and tailor treatment to your needs. The “new treatment for achalasia” in 2025 represents meaningful progress — but choices should be individualized.