Granuloma Annulare and Diabetes: Is There a Connection?
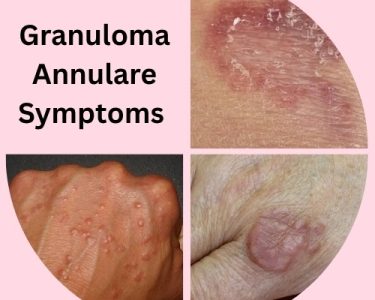
Granuloma annulare is a skin condition that often appears as ring-shaped, reddish bumps on the hands, feet, arms, or legs. For some people, this condition may appear without a clear cause. However, growing evidence shows a possible link between granuloma annulare and diabetes, particularly in chronic or generalised cases.
Many people ask if granuloma annulare is caused by high blood sugar. While not fully understood, researchers have noted that people with poorly controlled diabetes may be more likely to develop this skin disorder. In particular, diabetes granuloma annulare symptoms may appear more widespread and persistent compared to cases seen in people without diabetes.
Related Articles: What Causes Granuloma Annulare and How to Manage Flare-Ups
Evidence Supporting the Link:
- Generalized GA and Diabetes: Studies show a higher prevalence of diabetes in patients with generalized granuloma annulare compared to those with localized forms.
- Abnormal Glucose Tolerance: Some patients with GA who do not have a diabetes diagnosis may still exhibit impaired glucose tolerance or insulin resistance.
- Shared Inflammatory Pathways: Both diabetes and GA involve immune system activity and inflammation, which may play a role in their association.
Possible Mechanisms:
While the exact biological mechanism is unclear, potential theories include:
- Microvascular damage from chronic high blood sugar.
- Immunologic dysfunction triggered by diabetes.
- Collagen degeneration and abnormal immune responses affecting skin tissue.
Who Is at Risk?
Granuloma annulare can affect individuals of any age, but:
- Adults with type 2 diabetes are more commonly seen with the generalized form.
- Childrentypically present with localized or subcutaneous GA and are less likely to have diabetes.
- Womenare more frequently affected by GA than men.
How Diabetes Affects the Skin
People living with diabetes can experience a range of skin problems due to poor circulation, nerve damage, and elevated glucose levels. One of the lesser-known associations is granuloma annulare in diabetes. This skin condition may reflect long-term inflammation or immune changes triggered by high blood sugar.
In cases where blood sugar diabetes granuloma annulare coexists, the rash may resist typical treatments and remain for months or even years. It can also appear in unusual areas, such as the torso, and may be more prominent in people with Type 1 diabetes.
Who Is Most at Risk?
Studies suggest that granuloma annulare type 1 diabetesis more frequently seen in those diagnosed during childhood or adolescence. However, it can affect anyone whose blood glucose is poorly controlled. While not life-threatening, it may be a sign that blood sugar levels need to be addressed more effectively.
If you’ve noticed ring-like skin lesions and you live with diabetes, speak to your doctor. Identifying diabetes skin diabetes granuloma annulare early can support better overall management.
Recognising Diabetes Granuloma Annulare Symptoms
Look for:
Ring-shaped Lesions
- Most characteristic sign.
- Circular or arc-shaped patches.
- Typically have a raised border with a clear center.
Skin-colored or Reddish Bumps
- May be pink, purple, or flesh-toned.
- Can blend with surrounding skin or stand out visibly.
Widespread Distribution (Generalized Form)
- Common in people with diabetes.
- Lesions may appear on the trunk, arms, legs, and even hands or feet.
- More extensive than localized types.
Itching or Burning (Mild)
- Usually painless, but some people report mild itchiness or burning.
Chronic or Recurrent Nature
- Lesions may come and go over months or even years.
- May worsen with poorly controlled diabetes.
Granuloma Annulare vs. Diabetic Dermopathy
- Granuloma annulare is often confused with diabetic dermopathy, which causes small, round, brownish patches on the shins.
- However, granuloma annulare is raised, ring-shaped, and can be widespread, while diabetic dermopathy is flat, brown, and mostly on the lower legs.
People with diabetes and granuloma annulare may notice that the condition develops gradually and doesn’t disappear quickly. The skin changes can sometimes be mistaken for a fungal infection or eczema.
Diabetes Granuloma Annulare Treatment Options
There’s no single cure, but treatment often focuses on improving blood glucose control. In many cases, the rash improves as diabetes becomes better managed. Here’s how to approach diabetes granuloma annulare treatment:
Related Articles: What is the Best Treatment for Granuloma Annulare?
Below are the most commonly used treatment strategies.
1. Optimizing Diabetes Control
Primary strategy for managing granuloma annulare in diabetics is to control blood sugar levels effectively. Some cases have shown improvement or complete resolution of lesions after better glycemic control. Strategies include:
- Regular blood glucose monitoring
- Diet and lifestyle modifications
- Use of insulin or oral hypoglycemic agents
- Avoiding blood sugar spikes
Tight glucose control can not only reduce the severity of granuloma annulare but also prevent its recurrence.
2. Topical Corticosteroids
For localized lesions, topical corticosteroids are often the first-line treatment. These help reduce inflammation and flatten the lesions.
- High-potency corticosteroids like clobetasol may be prescribed
- Applied directly to lesions 1–2 times a day
- Occlusive dressings can improve absorption and efficacy
However, long-term use can cause skin thinning, so this treatment should be monitored.
3. Intralesional Corticosteroid Injections
For stubborn or larger lesions, intralesional steroid injections like triamcinolone acetonide can be effective. This involves injecting the corticosteroid directly into the lesion to reduce inflammation from within.
- Typically done every 3–6 weeks
- Can lead to significant lesion flattening
- Minimal systemic side effects
However, it may be painful and not suitable for extensive cases.
4. Systemic Treatments
For generalized or widespread granuloma annulare—more common in diabetic patients—systemic therapies may be needed.
a. Oral Corticosteroids
- Prednisone or similar medications may be prescribed
- Short-term treatment for severe flare-ups
- Risk of blood sugar elevation in diabetics, so must be used cautiously
b. Antimalarial Drugs (e.g., Hydroxychloroquine)
- Anti-inflammatory properties helpful in GA
- Requires regular eye exams due to risk of retinal toxicity
c. Dapsone
- Antibiotic with anti-inflammatory effects
- Blood monitoring required due to potential for hemolysis
d. Isotretinoin (Accutane)
- Usually used in acne but sometimes effective in granuloma annulare
- Not suitable for all patients, particularly women of childbearing age
e. Methotrexate
- Immunosuppressive medication
- Effective in severe, treatment-resistant cases
- Requires liver monitoring and blood tests
5. Phototherapy
Ultraviolet light therapy, particularly PUVA (psoralen plus UVA) and narrow-band UVB, has been shown to help in treating generalized granuloma annulare.
- Involves regular sessions (2–3 times a week)
- Can induce remission in some patients
- Side effects may include sunburn or increased skin aging
This is generally considered a second-line therapy and is mostly reserved for widespread disease.
6. Cryotherapy
Cryotherapy, or liquid nitrogen treatment, may be useful for small, isolated lesions.
- Causes destruction of tissue through freezing
- Simple outpatient procedure
- Risk of pigment changes and scarring
Cryotherapy is not recommended for large or generalized GA.
7. Natural and Home Remedies (Supportive)
Though evidence is limited, some natural options may help reduce inflammation and support skin healing:
Related Articles: 10 Natural Remedies for Granuloma Annulare
- Aloe Vera Gel– anti-inflammatory and soothing
- Coconut Oil– moisturizes skin and reduces itching
- Turmeric– has systemic anti-inflammatory benefits
- Vitamin D Supplements– for immune regulation
- Omega-3 Fatty Acids– supports skin health
Natural Remedies for Granuloma Annulare should only be used alongside medical treatments, not as replacements.
8. Biologic Therapies
In rare, treatment-resistant cases, biologic agentslike adalimumab (Humira) or etanercept (Enbrel)have shown promise.
- Target specific parts of the immune system
- Expensive and generally reserved for severe autoimmune-related cases
- Long-term safety and effectiveness for GA are still under investigation
Dermatologists often coordinate with diabetes specialists to create a care plan that treats both the skin and blood sugar levels together.
Final Thoughts
If you’re managing diabetes and have noticed strange skin changes, don’t ignore them. There may be a direct link between diabetes granuloma annulare and your blood glucose control. Proper diagnosis and care can help ease symptoms and improve quality of life.
Learn more about how granuloma annulare and diabetes relate and what steps you can take by exploring our dedicated resources on managing skin conditions in diabetes.